For the past 25 years, I've been secretly cutting my own hair. It started when I was in college and I had super thick waist-length hair. I initially intended to just give myself a slight trim, maybe an inch or two at the very most...but the smooth snip-snip of the scissors was ever so much fun! and addictive! It was really quite difficult to let go of the scissors, and 20 minutes later, I found myself sporting a jaunty chin-length bob.
I used to set up 2 mirrors--one in front of me, and one behind me--so that I could get a good view of the back of my head while trimming my hair. These days, I just use one mirror and I judge whether I'm cutting well by feeling the back of my head for uneven hair distribution. I snipped away at my hair last night, and for some bizarre reason, all of my clinic patients with psychiatric diagnoses have been complimenting my haircut today. Bipolar disorder with low back pain thought the shape framed my face nicely. Obsessive compulsive disorder with a sinus infection especially liked the way my bangs swayed liltingly to one side. Even the strange lady with panic disorder who was standing in the corner of the exam room crying and holding her left arm as if she were a bird with a broken wing told me my hair looked great. None of these patients had a primary care provider they could see for follow up.
I grew up in an era when everyone had a family doctor, and it is a constant puzzle to me when I see so many patients at our urgent care clinic who don't have a primary care provider but want to be treated for a chronic condition. Many patients feel they're "too healthy" to have a regular doctor; others complain about how long it takes to set up an appointment to establish care. I have encountered multiple patients with severe abdominal pain or pelvic pain who went to the ED and waited for a few hours while labs were drawn, then left the ED to seek medical attention at our urgent care clinic because they "got tired of waiting". Even though they were having excruciating pain and they could have had access to CT scans, MRIs, ultrasounds and stat lab results in the ED (none of which are available in urgent care), they left because they wanted to be seen "right away". Then they get upset when we direct them back to the ED because we can't provide the higher level of care that they need. Our healthcare system is broken, and none of it makes any sense, but at least the psychiatric patients really like my hair...
Thursday, December 08, 2011
Wednesday, November 16, 2011
85 Patients!!!
Most of the time, I enjoy my new job, but every now and then I have a truly horrifying day that takes the wind out of my sails. On Monday, I arrived at the clinic to find that I had been completely and inexplicably locked out of the computer network. While hordes of patients were piling up in the waiting room, I was on the phone with IT, desperately trying to log on to the network and then to the EMR. When I finally regained access to the EMR, I discovered that I could only log on using one specific computer and that I was mysteriously locked out of the computers in all of the exam rooms.
Much of the day went like this: 5 upper respiratory infections, low back pain, the EMR sends error messages telling me my password is invalid, I spend 20 minutes on the phone with IT trying to regain access to the EMR, I see 5 more upper respiratory infections, shoulder pain, 4 bladder infections, and I'm locked out of the EMR again, I spend 20 minutes on the phone with IT....lather, rinse, repeat.
By 8:30 pm, we had so many patients camped out in the waiting room, we had to divert some of them to a different urgent care clinic. It wasn't until 9:15 pm when the last patient left that I realized, in a sort of post-traumatic haze, that we had seen 85 patients. You heard me: 2 clinicians, 85 patients!
It wasn't all bad. There were certainly small triumphs, like removing a pedunculated growth (probably a small hemangioma) from a 14-yr-old's scalp--it had been present since birth, and the surrounding skin had gotten infected with impetigo, and it was such fun to watch her marvel over the newly smooth texture of her scalp after the procedure.
When I was in medical school, I developed coping mechanisms for stressful days on my 3rd and 4th year clinical rotations: my official theme song was Dean Martin's "Ain't That a Kick in the Head". On my PDA, I had video clips of my friends & family saying silly things like "I'll see you in hell!" and "I'd like to order a CBC, a BMP, and a glass of red wine" which would inevitably make me smile, even on bad call nights.
My coping mechanisms this winter are as follows: I've fashioned a tiny bracelet from 1/4" white elastic and, using iron-on transfer paper, decorated it with the phrase "Mischief managed!" which is what Harry Potter utters when he wants to close up the Marauder's Map at Hogwarts. It reminds me that, no matter how crazy my work day is, it does eventually come to an end. I've also been watching episodes of "Make It or Break It", an ABC Family drama about teenage girls who are elite gymnasts striving to make it to the 2012 Olympics. What I love about women's gymnastics is how the athletes get a big hug every time they complete a performance on the vault, the balance beam or the uneven bars. When I'm dreading the long commute to work, I imagine myself as a gymnastics girl in a shiny leotard, with glittery eye shadow and a fluffy hair scrunchy, with my coach and teammates yelling, "You can do it!", "You've got this!" and "Stick that landing!" from the sidelines. Silly, I know, but it does make me feel better.
Much of the day went like this: 5 upper respiratory infections, low back pain, the EMR sends error messages telling me my password is invalid, I spend 20 minutes on the phone with IT trying to regain access to the EMR, I see 5 more upper respiratory infections, shoulder pain, 4 bladder infections, and I'm locked out of the EMR again, I spend 20 minutes on the phone with IT....lather, rinse, repeat.
By 8:30 pm, we had so many patients camped out in the waiting room, we had to divert some of them to a different urgent care clinic. It wasn't until 9:15 pm when the last patient left that I realized, in a sort of post-traumatic haze, that we had seen 85 patients. You heard me: 2 clinicians, 85 patients!
It wasn't all bad. There were certainly small triumphs, like removing a pedunculated growth (probably a small hemangioma) from a 14-yr-old's scalp--it had been present since birth, and the surrounding skin had gotten infected with impetigo, and it was such fun to watch her marvel over the newly smooth texture of her scalp after the procedure.
When I was in medical school, I developed coping mechanisms for stressful days on my 3rd and 4th year clinical rotations: my official theme song was Dean Martin's "Ain't That a Kick in the Head". On my PDA, I had video clips of my friends & family saying silly things like "I'll see you in hell!" and "I'd like to order a CBC, a BMP, and a glass of red wine" which would inevitably make me smile, even on bad call nights.
My coping mechanisms this winter are as follows: I've fashioned a tiny bracelet from 1/4" white elastic and, using iron-on transfer paper, decorated it with the phrase "Mischief managed!" which is what Harry Potter utters when he wants to close up the Marauder's Map at Hogwarts. It reminds me that, no matter how crazy my work day is, it does eventually come to an end. I've also been watching episodes of "Make It or Break It", an ABC Family drama about teenage girls who are elite gymnasts striving to make it to the 2012 Olympics. What I love about women's gymnastics is how the athletes get a big hug every time they complete a performance on the vault, the balance beam or the uneven bars. When I'm dreading the long commute to work, I imagine myself as a gymnastics girl in a shiny leotard, with glittery eye shadow and a fluffy hair scrunchy, with my coach and teammates yelling, "You can do it!", "You've got this!" and "Stick that landing!" from the sidelines. Silly, I know, but it does make me feel better.
Thursday, November 10, 2011
Pattern Recognition
I recently saw a 36-yr-old female who had a 5-day history of vaginal irritation with a "burning" sensation. She was seen a few days earlier and given diflucan for a presumed yeast infection, but her condition had not improved. She told me, "It just really burns" and "When I try to pee, nothing comes out". Her UA and GC/CT were negative. On physical exam, her labia was erythematous and markedly swollen. I suddenly remembered the last time I saw a patient with a similarly swollen labia and the same complaint of dysuria and urinary retention: it was a 14-yr-old girl who had come to the pediatric ED where I was doing a residency rotation. We initially suspected cellulitis. She was in so much pain that conscious sedation was required for her pelvic exam. After a meticulous search, we finally found a vesicular lesion: it turned out this young girl had the worst case of genital herpes in the history of the universe.
I did manage to find one shallow ulcerated lesion on my 36-yr-old patient's perineum which I promptly swabbed for HSV culture. She was very skeptical about the provisional diagnosis of herpes, but she was willing to try taking acyclovir. A few days later, the culture came back positive for HSV-2.
I did manage to find one shallow ulcerated lesion on my 36-yr-old patient's perineum which I promptly swabbed for HSV culture. She was very skeptical about the provisional diagnosis of herpes, but she was willing to try taking acyclovir. A few days later, the culture came back positive for HSV-2.
Monday, October 31, 2011
Driving My Life Away
I'm very excited about finally starting my first permanent MD job. The lovely thing about urgent care is that patients generally present with just one or two medical problems. I will never complain about the following: lancing abscesses, suturing lacerations (I had to stitch across the vermilion border on a lip laceration recently!), removing a foreign body from someone's eye (the patient was a very skittish young man who kept twitching away from me and reflexively shutting his eyes, but I finally got the tiny brown speck after a saline eye wash and a few passes with a sterile cotton swab).
Aside from seeing multitudes of patients with viral respiratory infections who would have been better off staying home to rest, my only beef with this job is the commute: 55 minutes on I-5 to get to work, 55 minutes to get home. It would behoove me to invest in the Berlitz or Rosetta Stone Spanish language course on CD [conduzco mi vida lejos?] so I can learn while driving, and to start saving my pennies for a hybrid car, methinks.
Aside from seeing multitudes of patients with viral respiratory infections who would have been better off staying home to rest, my only beef with this job is the commute: 55 minutes on I-5 to get to work, 55 minutes to get home. It would behoove me to invest in the Berlitz or Rosetta Stone Spanish language course on CD [conduzco mi vida lejos?] so I can learn while driving, and to start saving my pennies for a hybrid car, methinks.
Friday, September 30, 2011
Hoh Hoh Hoh
The Hoh Rain Forest, which is part of the Olympic National Park, is truly a wonder of the Pacific Northwest. One of just a few temperate rain forests in the U.S., it encompasses 24 miles of low elevation forest along the Hoh River, and the average annual precipitation is an astonishing 12 to 14 feet of rain.
There are a couple of short trails that loop through the forest near the visitor's center (one of which was closed because the park rangers didn't want a family of Roosevelt elks to be disturbed), as well as the more hardcore 17 mile Hoh River Trail which leads to Glacier Meadows near Mount Olympus.
Maybe because of my lack of height, I find myself entranced by the intricate network of intertwined tree roots, especially evident in seedlings that begin their growth on top of fallen logs.
The high humidity, deep soil and mild temperatures contribute to the astounding size of the trees. I have the sneaking suspicion that if I fell down in the rain forest, moss would immediately start growing on me.
I would probably have to call for help from this phone booth...
There are a couple of short trails that loop through the forest near the visitor's center (one of which was closed because the park rangers didn't want a family of Roosevelt elks to be disturbed), as well as the more hardcore 17 mile Hoh River Trail which leads to Glacier Meadows near Mount Olympus.
Maybe because of my lack of height, I find myself entranced by the intricate network of intertwined tree roots, especially evident in seedlings that begin their growth on top of fallen logs.
The high humidity, deep soil and mild temperatures contribute to the astounding size of the trees. I have the sneaking suspicion that if I fell down in the rain forest, moss would immediately start growing on me.
I would probably have to call for help from this phone booth...
Thursday, September 22, 2011
Trying To Act Like A Professional
Imagine you're seeing a 58-yr-old patient in clinic for the first time who is having problems with chronic hip pain. He is very tan, and his weathered face slightly resembles Mel Brooks.
You are, of course, sympathetic to his pain, and you conduct a thorough exam which finds that his symptoms are consistent with a R hip bursitis with tenderness to palpation at the greater trochanter. You want to offer a steroid injection into the bursa for pain relief, but you are becoming increasingly more distracted by this patient's...hair.
He has amazingly shiny and very dark hair, styled in a manner that looks a bit like this wig, but in a much deeper shade of brown:
The distraction becomes overwhelming, and you step out of the room briefly, run into a colleague who looks at you quizzically, and, unable to suppress the inevitable burst of glee, you whisper furtively, "I've got a 58-yr-old male with Prince Valiant hair!"
You are, of course, sympathetic to his pain, and you conduct a thorough exam which finds that his symptoms are consistent with a R hip bursitis with tenderness to palpation at the greater trochanter. You want to offer a steroid injection into the bursa for pain relief, but you are becoming increasingly more distracted by this patient's...hair.
He has amazingly shiny and very dark hair, styled in a manner that looks a bit like this wig, but in a much deeper shade of brown:
The distraction becomes overwhelming, and you step out of the room briefly, run into a colleague who looks at you quizzically, and, unable to suppress the inevitable burst of glee, you whisper furtively, "I've got a 58-yr-old male with Prince Valiant hair!"
Saturday, September 17, 2011
Flattery Will Get You Everywhere
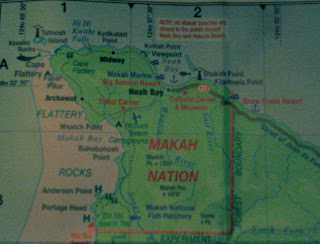
Cape Flattery is just 8 miles away, and it's known as the northwesternmost point of the contiguous United States. It was named in 1778 by British explorer Captain James Cook who noted from his ship, "there appeared to be a small opening which flattered us with the hopes of finding a harbour". The often muddy trail to the Cape is made less treacherous by strategic placement of cedar plank boardwalk constructed in 1996 by 7 members of the Makah tribe.
Once you get about halfway through the 3/4 mile trail, you start to hear the sound of the ocean, but you can't really tell where it's coming from until you approach the first observation deck.
There are 5 observation decks constructed with cedar planks and guard rails, with breathtaking views overlooking both the Pacific Ocean and the Strait of Juan de Fuca. You can see picturesque sea stacks with trees growing on top, sometimes populated by puffins. If you're lucky, you may catch otters sunning themselves on the rocks below.
Tatoosh Island, 1/2 mile off the coast from the Cape Flattery, is a former Makah fishing and whaling camp; the lighthouse on the island was built in 1857 and is owned & operated by the Coast Guard.
Once you get about halfway through the 3/4 mile trail, you start to hear the sound of the ocean, but you can't really tell where it's coming from until you approach the first observation deck.
There are 5 observation decks constructed with cedar planks and guard rails, with breathtaking views overlooking both the Pacific Ocean and the Strait of Juan de Fuca. You can see picturesque sea stacks with trees growing on top, sometimes populated by puffins. If you're lucky, you may catch otters sunning themselves on the rocks below.
Tatoosh Island, 1/2 mile off the coast from the Cape Flattery, is a former Makah fishing and whaling camp; the lighthouse on the island was built in 1857 and is owned & operated by the Coast Guard.
Also visible are a proliferation of sea caves which are dramatic openings worn into the cliffs by the constant pounding of the ocean waves. The entire experience of traveling through the forest, then suddenly being confronted by the stunning beauty of the coast is surprisingly emotional and awe-inspiring.
Friday, September 09, 2011
Blackberry Teeth and the Neah Bay Rumor Mill
Sometimes clinic staff will bring in a homemade treat to share with everyone. Today it was a beautiful and impressively large blackberry cobbler baked in a cast iron pan. Most of us managed to nibble on it intermittently throughout the morning, but it wasn't until 11:30 that the pharmacy assistant sidled up to me and whispered, "Everyone who ate the cobbler has blue teeth!" I surreptitiously glanced at my mouth in the nearest mirror, and lo & behold--my teeth had freakishly taken on the same shade as the blue sclera of osteogenesis imperfecta.
The nurse practitioner tells me that some of the older aunties of the town have been gossiping that Dr Chan "doesn't touch patients". I'm not sure what that means--could they be referring to my habit of donning latex gloves before coming into contact with bodily fluids (e.g. during a bimanual exam, while palpating a lesion on someone's buccal mucosa, or while lancing an abscess)?? Because that's called taking universal precautions. The lab tech joked that I should do trigger point injections by administering the lidocaine & kenalog via blowdart, instead of the usual syringe with 27-gauge needle, so I can continue "not touching patients".
The nurse practitioner tells me that some of the older aunties of the town have been gossiping that Dr Chan "doesn't touch patients". I'm not sure what that means--could they be referring to my habit of donning latex gloves before coming into contact with bodily fluids (e.g. during a bimanual exam, while palpating a lesion on someone's buccal mucosa, or while lancing an abscess)?? Because that's called taking universal precautions. The lab tech joked that I should do trigger point injections by administering the lidocaine & kenalog via blowdart, instead of the usual syringe with 27-gauge needle, so I can continue "not touching patients".
Tuesday, September 06, 2011
Escape to Victoria
I can't imagine what it's like to be one of only two full-time permanent doctors in a remote rural community, constantly being on call and rarely taking time off. One of the doctors has been here for 7 years, and he's familiar with all the idiosyncracies of our more--shall we say?--eccentric clinic patients; he's a proponent of kickin' it old school, meaning that he still spends the whole day in clinic after being on call the night before. He enjoys canning salmon by dividing the fish to fit half-pint mason jars to stew for 100 minutes in a pressure cooker. The result is surprisingly fresh and has a shelf life of two years. The other doctor is about a year out of residency (like me) with additional training in acupuncture and other types of alternative medicine, which is wonderful for the abundance of patients with chronic pain. So many people who work in the commercial fishing industry don't have time to drive 60 miles & back to see the nearest physical therapist, but they're willing to try a 15 to 20 minute session of acupuncture in the clinic.
Over Labor Day weekend, I drove to Port Angeles and hopped a ferry to Vancouver Island where I was absolutely delighted to eat gelato in a waffle cone (for breakfast!), catch an afternoon of the Vancouver Island Blues Bash, tour the Butchart Gardens, and just stroll around marveling at the architecture of the faintly Anglophilic city of Victoria, British Columbia.
Over Labor Day weekend, I drove to Port Angeles and hopped a ferry to Vancouver Island where I was absolutely delighted to eat gelato in a waffle cone (for breakfast!), catch an afternoon of the Vancouver Island Blues Bash, tour the Butchart Gardens, and just stroll around marveling at the architecture of the faintly Anglophilic city of Victoria, British Columbia.
 |
| The Empress Fairmont, where High Tea is served |
 |
| The Legislative Building, where the government lives |
 |
| The Japanese Garden at Butchart Gardens |
Saturday, August 27, 2011
These Boots Were Made For Walk-Ins
The clinic has 6 exam rooms and 1 small trauma room which is often used for minor accidents, since the closest hospital is 60 miles away in Forks (the land of Twilight aficionados). Most of the visits are walk-ins, and after a while it all blurs together at a very brisk pace: from the woman who marched into the waiting room demanding "PowerPoint injections" for bilateral elbow pain (I'll call Microsoft, stat! I thought to myself) to the young man who sheepishly admitted his chief complaint wasn't coughing, as he told the nurse, but actually a 3-day history of green penile discharge (Condoms! I croaked, while injecting him with ceftriaxone and making him swallow 1 gram of azithromycin)...at the end of the day, I'm usually dazed and hypoglycemic--that is, if I'm not too busy cursing the cumbersome Cro-Magnon era EMR.
I had the opportunity to use the trauma room yesterday when we received a radio report about a grass fire, which turned out to be a man on the grass who was on fire. The town was hit with an influx of visitors for the Makah Days Festival, a celebration of Makah culture involving canoe races, traditional dancing, vendors, a talent show, and a salmon bake. In the midst of all the excitement, a large barrel of heated roofing tar spontaneously combusted, and the patient sustained 2nd degree burns on his R hand and R leg. The EMTs brought him in on high-flow oxygen with a nonrebreather mask, already hooked up by IV to a 1-liter bag of normal saline. Although his nasal mucosa was mildly singed, he was breathing normally with no signs of airway edema. The blisters on his skin were starting to pop, and we debrided quite a bit of the dead skin from the burns.
After all the drama, I was able to slip away quietly this morning to meet up with my brother & his family who were camping 54 miles away at the Olympic National Park. We took a trip to La Push to spend the day at Rialto Beach which has a wildly beautiful rocky shoreline punctuated with silvery driftwood that has been tempered by centuries of ocean waves to look quite sculptural.

I had the opportunity to use the trauma room yesterday when we received a radio report about a grass fire, which turned out to be a man on the grass who was on fire. The town was hit with an influx of visitors for the Makah Days Festival, a celebration of Makah culture involving canoe races, traditional dancing, vendors, a talent show, and a salmon bake. In the midst of all the excitement, a large barrel of heated roofing tar spontaneously combusted, and the patient sustained 2nd degree burns on his R hand and R leg. The EMTs brought him in on high-flow oxygen with a nonrebreather mask, already hooked up by IV to a 1-liter bag of normal saline. Although his nasal mucosa was mildly singed, he was breathing normally with no signs of airway edema. The blisters on his skin were starting to pop, and we debrided quite a bit of the dead skin from the burns.
After all the drama, I was able to slip away quietly this morning to meet up with my brother & his family who were camping 54 miles away at the Olympic National Park. We took a trip to La Push to spend the day at Rialto Beach which has a wildly beautiful rocky shoreline punctuated with silvery driftwood that has been tempered by centuries of ocean waves to look quite sculptural.

When I arrived back at Neah Bay just as the sun was setting, I found the entire town shrouded in fog and the main road blocked off by an ambulance, a fire truck, and 2 police cars. Which somehow did not surprise me...
Thursday, August 18, 2011
Neah Bay
 |
| Goodbye, Space Needle! |
 |
| Hello, Bainbridge Island! |
 |
| The shoreline in Neah Bay |
 |
| The Makah Marina |
Whaling was a significant part of ancient Makah tradition, and the tribal logo is a reference to an old legend about a thunderbird delivering a whale to the Makah people during a time of starvation:
You can see representations of this legend in various forms around town:
My temporary home for the next 6 weeks or so is across the street from the police station and jail:
In fact, one of my first clinic patients was a young man in a bright orange jumpsuit, sporting handcuffs and accompanied by a guard. He had pain in both of his forearms, most likely a repetitive stress injury from lifting 60-lb baskets of fish the day before. I suggested releasing the young man ever so briefly from the handcuffs so I could conduct a more thorough exam. This, according to the guard, was not possible. I explained that the repetitive stress injury would resolve faster if the young inmate was allowed to rest from the aggravating activity. The guard shot me a look as if to say, Lady, have you completely lost your marbles?! Apparently there is no rest for the wicked.
Thursday, August 11, 2011
Fly Away With Me
My final night float elicited all kinds of excitement:
-A 77-yr-old woman who had collapsed and was found to have a blood glucose level of 12! After several amps of D50, her blood sugar increased temporarily to 70, then precipitously dropped again. I started her on an intravenous infusion of D10, then ordered some extra D50 for back-up. Turns out the hospital was running low on D50 and had to reserve a few amps for the crash carts. Meanwhile, the patient's blood sugar dropped to 41 despite the D10. Theory: I'm guessing she took some "extra" doses of her extended release glipizide--an insulin secretagogue that can take quite a while to metabolize completely in elderly patients. I ordered glucagon to be administered every time her blood sugar level dropped to the 50s. After 6 or 7 doses, we finally got a blood glucose reading of 124 which fell a bit to 90 an hour later, but managed to stay consistently above 75. By which time, the patient was alert enough to drink juice when prompted.
-A 13-yr-old boy with an impressively large R knee laceration after taking a tumble off his skateboard. The gaping wound revealed some subcutaneous tissue which astounded his parents. You know you're among hunters when the most frequent remark about large lacerations is: "You can see the meat sticking out!" As I was carefully suturing the laceration (13 stitches total), the boy pulled a tiny replica of a skateboard out of his pocket to reenact the scene of the accident for me.
-A cab driver with posterior epistaxis that had been bleeding nonstop for 2 hours, complicated by hypertensive urgency with systolic blood pressures in the 180s. He got a double lumen balloon catheter inserted into his right nasal cavity for tamponade, and several doses of IV labetalol for his blood pressure. Ultimately, he would need to fly to Anchorage for definitive treatment by an ENT specialist.
The funny thing about coming off of night float and taking the morning flight back to Seattle is that almost inevitably you end up on the same Bethel-Anchorage flight as some of your patients! On my flight, I spotted the woman who had the breech delivery in the village (on her way to the NICU in Anchorage to see her newborn), and a little girl who had been treated for R cheek cellulitis secondary to an odontogenic abscess (scheduled for oral surgery in Anchorage later that day). If only the cab driver with the nosebleed had driven us all to the airport and hopped on the flight with us, it would have been a perfect trifecta.
-A 77-yr-old woman who had collapsed and was found to have a blood glucose level of 12! After several amps of D50, her blood sugar increased temporarily to 70, then precipitously dropped again. I started her on an intravenous infusion of D10, then ordered some extra D50 for back-up. Turns out the hospital was running low on D50 and had to reserve a few amps for the crash carts. Meanwhile, the patient's blood sugar dropped to 41 despite the D10. Theory: I'm guessing she took some "extra" doses of her extended release glipizide--an insulin secretagogue that can take quite a while to metabolize completely in elderly patients. I ordered glucagon to be administered every time her blood sugar level dropped to the 50s. After 6 or 7 doses, we finally got a blood glucose reading of 124 which fell a bit to 90 an hour later, but managed to stay consistently above 75. By which time, the patient was alert enough to drink juice when prompted.
-A 13-yr-old boy with an impressively large R knee laceration after taking a tumble off his skateboard. The gaping wound revealed some subcutaneous tissue which astounded his parents. You know you're among hunters when the most frequent remark about large lacerations is: "You can see the meat sticking out!" As I was carefully suturing the laceration (13 stitches total), the boy pulled a tiny replica of a skateboard out of his pocket to reenact the scene of the accident for me.
-A cab driver with posterior epistaxis that had been bleeding nonstop for 2 hours, complicated by hypertensive urgency with systolic blood pressures in the 180s. He got a double lumen balloon catheter inserted into his right nasal cavity for tamponade, and several doses of IV labetalol for his blood pressure. Ultimately, he would need to fly to Anchorage for definitive treatment by an ENT specialist.
The funny thing about coming off of night float and taking the morning flight back to Seattle is that almost inevitably you end up on the same Bethel-Anchorage flight as some of your patients! On my flight, I spotted the woman who had the breech delivery in the village (on her way to the NICU in Anchorage to see her newborn), and a little girl who had been treated for R cheek cellulitis secondary to an odontogenic abscess (scheduled for oral surgery in Anchorage later that day). If only the cab driver with the nosebleed had driven us all to the airport and hopped on the flight with us, it would have been a perfect trifecta.
Tuesday, August 09, 2011
Night of Incredibly Bad OB Mojo
My night float started off with a 24 yr old G1 P0 at 36 + 2/7 wks with her baby in footling breech position, having contractions every 5 minutes, cervix dilated to 2 cm and 60% effaced. We gave her IM terbutaline, but 90 minutes later she had made more cervical change, so high-risk OB came in to attempt an extraversion (to turn the baby around so s/he would be in head-down position). Which failed. Which led to an uneventful C-section that went very well.
After completing several ER admissions (including a 32-yr-old male in diabetic ketoacidosis who was not very compliant with his daily lantus regimen and whose last known HbA1c was a whopping 15.9%; and a tiny 82-yr-old woman with dementia, visual hallucinations, and a 4-night run of insomnia, who promptly fell asleep after 1 mg of haldol) I got a phone call from the village of Emmonak.
Things you never want to hear a health aide say:
1. This woman is having contractions every 3 minutes and she says she's 38 weeks pregnant, but I think she's only 30 weeks pregnant: The patient had no prenatal care for this pregnancy and we had no reliable records of her LMP or even of a positive urine pregnancy test. I started to activate a medevac, thinking that the on-call pediatrician & I would have to fly out to Emmonak for the delivery. I checked her old medical chart and found out she had no history of preterm delivery, just one baby delivered at 37 weeks in 2009.
2. I think her cervix is completely open and I think I can feel the baby's nose: This is a very bad sign that the delivery is imminent and the presenting part is not the head. There's no way the pediatrician & I can get to the village in time.
3. She started pushing, and I think a foot is coming out of her vagina: OMG, it's another footling breech! The health aide had me on speaker phone as I coached him through the breech delivery.
4. The baby is out but he's not breathing: The pediatrician took over the speaker phone and started coaching the health aide & his helpers through the process of neonatal resuscitation.
5. It's been almost 50 minutes and the placenta hasn't come out yet: By this time, the baby was doing better and the pediatrician was en route to Emmonak with the flight crew. The health aide was trying to get pitocin started, as his helpers were applying gentle traction on the umbilical cord and massaging the fundus.
6. Do you think the medevac flight is bringing blood for transfusion?: The health aide estimated a total blood loss of one liter and the mother was still bleeding. The placenta finally came out, and I had the health aide insert his hand in the uterus and manually extract several blood clots and a possible fragment of placenta. I could hear the mother screaming in the background on speaker phone. The only medication for postpartum hemorrhage in the village clinic was methergine which I was hoping not to use. The bleeding finally trickled to a halt, and I had them run IVF at full speed, given mother's tachycardia of 120 bpm.
Meanwhile, I was paged for an OB patient who presented with intractable vomiting, coffee ground emesis and one episode of emesis containing bright red blood, after she drank an entire bottle of R&R the day before. She had been drinking through her entire first trimester, stopped for most of her second trimester, and was now at 26 weeks. I wrote for IV zofran alternating with PR phenergan, then a loading dose of protonix 80 mg by IV, followed by a protonix drip at 8mg/hr to stop the GI bleed. When she complained of epigastric pain, I ordered the magic "GI cocktail" (10cc each of maalox, viscous lidocaine, and benadryl) which soothed her and put her to sleep almost immediately.
Shortly before change of shift, I got a call from the village of Napaskiak: a G3P1 at 34 + 4/7 wks (with excellent dates by 10-wk ultrasound) was having contractions every 3 minutes. After 2 doses of IM terbutaline and a liter of normal saline, the contractions had spaced out a little and were much shorter and less intense. The health aide tried to check the cervix for dilation: "I put my entire hand up there as far as it could go and I still didn't feel anything, " which is a good sign. I spoke with high-risk OB and we agreed to have the pt come to Bethel by boat (just a short 30 minute ride) for further evaluation.
Then I went home and fell, exhausted, into bed.
After completing several ER admissions (including a 32-yr-old male in diabetic ketoacidosis who was not very compliant with his daily lantus regimen and whose last known HbA1c was a whopping 15.9%; and a tiny 82-yr-old woman with dementia, visual hallucinations, and a 4-night run of insomnia, who promptly fell asleep after 1 mg of haldol) I got a phone call from the village of Emmonak.
Things you never want to hear a health aide say:
1. This woman is having contractions every 3 minutes and she says she's 38 weeks pregnant, but I think she's only 30 weeks pregnant: The patient had no prenatal care for this pregnancy and we had no reliable records of her LMP or even of a positive urine pregnancy test. I started to activate a medevac, thinking that the on-call pediatrician & I would have to fly out to Emmonak for the delivery. I checked her old medical chart and found out she had no history of preterm delivery, just one baby delivered at 37 weeks in 2009.
2. I think her cervix is completely open and I think I can feel the baby's nose: This is a very bad sign that the delivery is imminent and the presenting part is not the head. There's no way the pediatrician & I can get to the village in time.
3. She started pushing, and I think a foot is coming out of her vagina: OMG, it's another footling breech! The health aide had me on speaker phone as I coached him through the breech delivery.
4. The baby is out but he's not breathing: The pediatrician took over the speaker phone and started coaching the health aide & his helpers through the process of neonatal resuscitation.
5. It's been almost 50 minutes and the placenta hasn't come out yet: By this time, the baby was doing better and the pediatrician was en route to Emmonak with the flight crew. The health aide was trying to get pitocin started, as his helpers were applying gentle traction on the umbilical cord and massaging the fundus.
6. Do you think the medevac flight is bringing blood for transfusion?: The health aide estimated a total blood loss of one liter and the mother was still bleeding. The placenta finally came out, and I had the health aide insert his hand in the uterus and manually extract several blood clots and a possible fragment of placenta. I could hear the mother screaming in the background on speaker phone. The only medication for postpartum hemorrhage in the village clinic was methergine which I was hoping not to use. The bleeding finally trickled to a halt, and I had them run IVF at full speed, given mother's tachycardia of 120 bpm.
Meanwhile, I was paged for an OB patient who presented with intractable vomiting, coffee ground emesis and one episode of emesis containing bright red blood, after she drank an entire bottle of R&R the day before. She had been drinking through her entire first trimester, stopped for most of her second trimester, and was now at 26 weeks. I wrote for IV zofran alternating with PR phenergan, then a loading dose of protonix 80 mg by IV, followed by a protonix drip at 8mg/hr to stop the GI bleed. When she complained of epigastric pain, I ordered the magic "GI cocktail" (10cc each of maalox, viscous lidocaine, and benadryl) which soothed her and put her to sleep almost immediately.
Shortly before change of shift, I got a call from the village of Napaskiak: a G3P1 at 34 + 4/7 wks (with excellent dates by 10-wk ultrasound) was having contractions every 3 minutes. After 2 doses of IM terbutaline and a liter of normal saline, the contractions had spaced out a little and were much shorter and less intense. The health aide tried to check the cervix for dilation: "I put my entire hand up there as far as it could go and I still didn't feel anything, " which is a good sign. I spoke with high-risk OB and we agreed to have the pt come to Bethel by boat (just a short 30 minute ride) for further evaluation.
Then I went home and fell, exhausted, into bed.
Sunday, August 07, 2011
There's Not Enough Room In This Town For You & Me & All That Pus
Skin infections appear to be running rampant on the wards this week:
-an affable 56-yr-old man who accidentally knelt on a nail while working on his fishing boat and ended up with an abscess on his R knee and extensive cellulitis from thigh to mid-shin.
-a very tired-appearing 47-yr-old woman who had incision & drainage of an abscess on her R upper back, then developed a severe allergic reaction (enormous hives and swelling which required an H1-blocker, an H2-blocker, epinephrine and prednisone) to the antibiotic she was prescribed. Several days later, the infection evolved into a rapidly-spreading cellulitis running from her upper back to the RLQ of her abdominal wall
-a 7-yr-old child with pus seeping out of an infected occipital laceration
60% of the RMT calls this week have been about abscesses and cellulitis. It's hard to fight skin infections in the villages when people live in rather close quarters and some houses don't have running water. Many people are thoroughly repulsed by pus. Call me morbid, but I find it very satisfying to open up an abscess with a #11 scalpel and release a gush of suppurative fluid...
-an affable 56-yr-old man who accidentally knelt on a nail while working on his fishing boat and ended up with an abscess on his R knee and extensive cellulitis from thigh to mid-shin.
-a very tired-appearing 47-yr-old woman who had incision & drainage of an abscess on her R upper back, then developed a severe allergic reaction (enormous hives and swelling which required an H1-blocker, an H2-blocker, epinephrine and prednisone) to the antibiotic she was prescribed. Several days later, the infection evolved into a rapidly-spreading cellulitis running from her upper back to the RLQ of her abdominal wall
-a 7-yr-old child with pus seeping out of an infected occipital laceration
60% of the RMT calls this week have been about abscesses and cellulitis. It's hard to fight skin infections in the villages when people live in rather close quarters and some houses don't have running water. Many people are thoroughly repulsed by pus. Call me morbid, but I find it very satisfying to open up an abscess with a #11 scalpel and release a gush of suppurative fluid...
Friday, August 05, 2011
Jackie Chan, Meet Dr Chan
"Everyone thinks I look like Jackie Chan," says my 52-yr-old patient who was admitted for dilantin toxicity. Only he makes it infinitely more amusing by swooping into a karate chop gesture every time he says "Jackie Chan". Which is quite frequent.
This delightful patient has a seizure disorder for which he takes dilantin and valproic acid. He has a special mantra to remind himself how many tablets of valproic acid to take: "Five in the morning, six at night, no whiskey". I suspect he accidentally used the valproic acid mantra with his dilantin tablets and ended up with a supratherapeutic serum dilantin level.
Our Jackie Chan lookalike also has an oddly low serum sodium level which dipped down to 123 without any apparent neurological symptoms. I was able to get his serum sodium to climb up to 128 (still low) with a bit of intravenous 0.9% saline. With a urine sodium >40 and a slightly low serum osmolality, he probably has SIADH, which is often treated with free water restriction and oral salt tablets. It's the antithesis of what we usually tell our patients: Drink less fluid! Use at least a 1/2 teaspoon of salt with all your meals! The hospital is on a "healthy eating" kick and has substituted all salt packets with Mrs Dash's Salt Substitute. I had to rummage through 3 different staff break rooms before I finally unearthed a plastic container brimming with contraband salt packets. After I sprinkled his scrambled egg breakfast with one of the salt packets, my patient grinned and said, "My brother looks like Mr Miyagi."
This delightful patient has a seizure disorder for which he takes dilantin and valproic acid. He has a special mantra to remind himself how many tablets of valproic acid to take: "Five in the morning, six at night, no whiskey". I suspect he accidentally used the valproic acid mantra with his dilantin tablets and ended up with a supratherapeutic serum dilantin level.
Our Jackie Chan lookalike also has an oddly low serum sodium level which dipped down to 123 without any apparent neurological symptoms. I was able to get his serum sodium to climb up to 128 (still low) with a bit of intravenous 0.9% saline. With a urine sodium >40 and a slightly low serum osmolality, he probably has SIADH, which is often treated with free water restriction and oral salt tablets. It's the antithesis of what we usually tell our patients: Drink less fluid! Use at least a 1/2 teaspoon of salt with all your meals! The hospital is on a "healthy eating" kick and has substituted all salt packets with Mrs Dash's Salt Substitute. I had to rummage through 3 different staff break rooms before I finally unearthed a plastic container brimming with contraband salt packets. After I sprinkled his scrambled egg breakfast with one of the salt packets, my patient grinned and said, "My brother looks like Mr Miyagi."
Wednesday, August 03, 2011
Bethel, We've Got To Stop Meeting Like This
This is my last foray to rural Alaska before I start my new job in October, and I'm still amazed by the lovely greenness of summer. All of my familiar icy landmarks have melted away into an unrecognizably verdant landscape of tall grass and bushes.
Some of the hospital patients, however, remain a little too familiar--for instance, the 49-yr-old woman who is frequently admitted for one of two reasons: alcohol intoxication or alcohol withdrawal. She was just discharged last week, and she bounced back onto my service yesterday. After multiple doses of ativan and haldol administered at regular intervals, the patient woke up this morning requesting a shower. She was in that very narrow window between intoxication and withdrawal where she was fairly lucid and cooperative. Hold her any longer and she goes into a full-blown and very unpleasant withdrawal. Let her go and she finds enough alcohol to keep herself adequately inebriated to avoid withdrawal. Since she has never shown any interest in detox or any other treatment, I discharged her and kept my fingers crossed that she would stay out of trouble for at least another week or two. She beamed at me, looking rather raccoon-ish with her bilateral periorbital contusions, and I couldn't help smiling back at her.
Some of the hospital patients, however, remain a little too familiar--for instance, the 49-yr-old woman who is frequently admitted for one of two reasons: alcohol intoxication or alcohol withdrawal. She was just discharged last week, and she bounced back onto my service yesterday. After multiple doses of ativan and haldol administered at regular intervals, the patient woke up this morning requesting a shower. She was in that very narrow window between intoxication and withdrawal where she was fairly lucid and cooperative. Hold her any longer and she goes into a full-blown and very unpleasant withdrawal. Let her go and she finds enough alcohol to keep herself adequately inebriated to avoid withdrawal. Since she has never shown any interest in detox or any other treatment, I discharged her and kept my fingers crossed that she would stay out of trouble for at least another week or two. She beamed at me, looking rather raccoon-ish with her bilateral periorbital contusions, and I couldn't help smiling back at her.
Thursday, July 21, 2011
Fog, Glorious Fog!
Having recently returned from a CME on hospitalist procedures in San Francisco, I must admit I kind of miss the fog that often rolls in as evening falls. A lot has changed in my favorite town since I moved away, but many things remain the same. Between practice sessions spent mastering the insertion of central venous lines in the right IJ and right subclavian veins of anatomical models (you know you hit the right spot when your finder needle aspirates windex-blue fluid), I was able to hop on the 38 Geary bus which whisked me away from Union Square and rolled all the way down to Land's End, where I took a lovely stroll by the Pacific Ocean during low tide.
Saturday, July 02, 2011
Snip Snip
Have you ever completed a vaginal laceration repair shortly after a successful delivery, wondered, "Why is there a bandaid on this patient's R buttock?", and removed the bandaid (which was starting to peel off anyway), only to find a growth that resembles a small penile glans? The texture was a cross between a stale marshmellow and a lipoma. The patient's PMD had been reluctant to remove the growth, fearing it might be highly vascularized. I anesthetized the skin around the lesion with a field block of 1% lidocaine with epinephrine, stuck a needle in it, and when no giant geyser of blood erupted, performed an excisional biopsy and sent the odd growth to pathology for further evaluation.
Friday, July 01, 2011
When All Else Fails, Hold A Sleeping Baby
One of the Yup'ik elders on my service has the dwindles. He's 87, he has Lewy body dementia, and he has slowly been losing his strength and mobility over the past several months. He was originally admitted for acute R gluteal pain that radiated down his leg, likely secondary to a herniated disc at L4-L5; but he soon stopped eating and drinking altogether. He has an amazingly large and caring family, all of whom are deeply invested in his well-being. I have had numerous conversations with his siblings, adult children and adult grandchildren about his prognosis all week. We had a family conference by speaker phone yesterday so that family here at the hospital could communicate en masse with family back home in the village. The ones who had been in Bethel all week by his bedside felt strongly that he should go home to familiar surroundings. The ones in the home village were less certain and wanted to try more aggressive interventions (i.e. artificial nutrition by NG tube) in the hospital. The patient's sons were on their way home from fish camp (everyone sets up fish camp by the river in the summertime, in order to catch and then slowly dry an adequate supply of salmon and herring to last throughout the winter).
This morning, it was decided that the patient would go home to be cared for by family. I put in a special request for a "reverse medevac" because he was too weak to sit up for a commercial flight home. An Expected Home Death form was filed in his chart. When the paramedics finally arrived (the flight time had been delayed several times due to regular medevac requests that pre-empted the reverse medevac), we all got a little teary-eyed. The family graciously thanked me, and there were hugs all around.
After the plane took off, I tiptoed to L&D and sat quietly in a rocking chair for a few minutes, holding the baby I had delivered the day before, which somehow made me feel just a little bit better.
This morning, it was decided that the patient would go home to be cared for by family. I put in a special request for a "reverse medevac" because he was too weak to sit up for a commercial flight home. An Expected Home Death form was filed in his chart. When the paramedics finally arrived (the flight time had been delayed several times due to regular medevac requests that pre-empted the reverse medevac), we all got a little teary-eyed. The family graciously thanked me, and there were hugs all around.
After the plane took off, I tiptoed to L&D and sat quietly in a rocking chair for a few minutes, holding the baby I had delivered the day before, which somehow made me feel just a little bit better.
Thursday, June 30, 2011
Implanon Is My New Best Friend
Listen up, teenage girls of the Yukon-Kuskokwim Delta region: birth control is a really, really useful thing! Yes, I am talking to you, teenage primip being induced at 42 + 1/7 wks for postdates and oligohydramnios, crying between pushes. And you too, 18-yr-old girl admitted for a septic abortion at 8 weeks EGA, getting IV doxycycline and unasyn.
Last night, I had a very long talk with the 18-yr-old about the pros and cons of all the birth control methods available in the universe and gave her a detailed educational handout with tiny pictures of everything we discussed. This morning, she told the nurse, "I want my birth control. When can I have it?". Asked which method she had chosen, she replied, "The poke." Poking could describe either the depo provera injection that's good for 3 months, or the implanon implants that are good for 3 years. Luckily, she chose the fantastically low maintenance implanon which was inserted posthaste just before she was discharged home.
Last night, I had a very long talk with the 18-yr-old about the pros and cons of all the birth control methods available in the universe and gave her a detailed educational handout with tiny pictures of everything we discussed. This morning, she told the nurse, "I want my birth control. When can I have it?". Asked which method she had chosen, she replied, "The poke." Poking could describe either the depo provera injection that's good for 3 months, or the implanon implants that are good for 3 years. Luckily, she chose the fantastically low maintenance implanon which was inserted posthaste just before she was discharged home.
Wednesday, June 29, 2011
Dishes Are Dangerous
My pager goes off incessantly, and it's hard to predict whether it's the ER doc asking me to admit a sick child, a village health aide asking what to do about a man whose right index finger is almost completely severed after getting his hand caught in a flywheel, or the lab calling to report a sky-high INR value of 18. When I saw the page from OB this afternoon, I assumed that my 23-yr-old G7P2 being induced for cholestasis of pregnancy was on the verge of delivering...but it was actually one of the OB nurses who whispered sotte voce: "This is not urgent, but I cut my thumb and I was wondering if you would take a look at it." She had been washing dishes and accidentally shattered a mug, producing a curvilinear laceration that crossed the PIP joint of her left thumb. The bleeding had stopped after she applied pressure, and her range of motion was perfectly preserved. "Do you think I need stitches, or can I just keep it wrapped up in a bandage?"
Because of the awkward position of the laceration over a joint, I decided to give her a few stitches to hold the wound edges together during the healing process. One of the other OB nurses broke into the surgical wing and gleefully returned with 4-0 nylon suture, 1% lidocaine with epinephrine, Adson forceps, and the most beautiful, delicate needle driver I have ever seen. "It's a Webster," she told me. "It costs $300." It took all of my willpower not to surreptitiously sneak it into one of the myriad pockets on my scrubs. In the end, the injured nurse got 3 stitches and we all agreed she had to fabricate a far more swashbuckling explanation for the mechanism of her injury.
Because of the awkward position of the laceration over a joint, I decided to give her a few stitches to hold the wound edges together during the healing process. One of the other OB nurses broke into the surgical wing and gleefully returned with 4-0 nylon suture, 1% lidocaine with epinephrine, Adson forceps, and the most beautiful, delicate needle driver I have ever seen. "It's a Webster," she told me. "It costs $300." It took all of my willpower not to surreptitiously sneak it into one of the myriad pockets on my scrubs. In the end, the injured nurse got 3 stitches and we all agreed she had to fabricate a far more swashbuckling explanation for the mechanism of her injury.
Tuesday, June 28, 2011
Of Maggots And Mental Status Exams
My most entertaining patient is a 67-yr-old monolingual Yup'ik-speaking man admitted for weeping ulcers on his lower extremities that were infested with maggots. His legs are completely discolored with thick layers of exfoliating skin. He has had several amputations due to severe frostbite: he is missing 2 toes from his left foot, 1 toe from his right foot, and 4 fingers from his right hand. Despite all of these physical quirks, he is frequently smiling and joking. A young man from the patient's household is accompanying him during this hospitalization, but displays a curious lack of knowledge about the patient's baseline level of functioning ("I don't know, I just got out of jail" is his standard answer to our inquiries). On his second day of hospitalization, the patient's primary caretaker called to tell us that she can't take care of him anymore (not that she was taking particularly good care of him to begin with, given the maggots on his legs).
Patient (via Yup'ik interpreter): Was she drunk when she called? Because she always talks like that when she's been drinking.
To be fair, the patient's lower extremity ulcers are healing quite nicely now, possibly because of the neat work of the maggots: they're quite adept at digesting rotting organic material. The hospital social worker is filing an Adult Protective Services report for elder neglect, and she asked me to conduct a mental status exam to facilitate the patient's placement in a nursing home.
Here's my dilemma: the traditional Folstein MMSE is a 30-point questionnaire often used to screen for dementia. Questions include asking the patient to spell "world" backwards, to subtract 7 from 100 and keep subtracting 7 serially from the resulting answer, and to name the year/month/date/weekday. Are these questions appropriate for a patient who doesn't speak English and has limited exposure to formal education? I looked at the Mini-Cog Assessment Instrument for Dementia which is supposedly valid regardless of culture and educational status, but one of the items asks the patient to draw the face of a clock, then draw in hands to set the time to "10 minutes past 11 o'clock". Is this relevant to someone who lives in a remote village in rural southwestern Alaska and uses the position of the sun and the moon to tell time?
Patient (via Yup'ik interpreter): These questions are making my legs itch.
You & me both, baby...
Patient (via Yup'ik interpreter): Was she drunk when she called? Because she always talks like that when she's been drinking.
To be fair, the patient's lower extremity ulcers are healing quite nicely now, possibly because of the neat work of the maggots: they're quite adept at digesting rotting organic material. The hospital social worker is filing an Adult Protective Services report for elder neglect, and she asked me to conduct a mental status exam to facilitate the patient's placement in a nursing home.
Here's my dilemma: the traditional Folstein MMSE is a 30-point questionnaire often used to screen for dementia. Questions include asking the patient to spell "world" backwards, to subtract 7 from 100 and keep subtracting 7 serially from the resulting answer, and to name the year/month/date/weekday. Are these questions appropriate for a patient who doesn't speak English and has limited exposure to formal education? I looked at the Mini-Cog Assessment Instrument for Dementia which is supposedly valid regardless of culture and educational status, but one of the items asks the patient to draw the face of a clock, then draw in hands to set the time to "10 minutes past 11 o'clock". Is this relevant to someone who lives in a remote village in rural southwestern Alaska and uses the position of the sun and the moon to tell time?
Patient (via Yup'ik interpreter): These questions are making my legs itch.
You & me both, baby...
Monday, June 27, 2011
Back in Bethel
If you're wondering what Bethel, Alaska looks like without all that ice and snow, look no further: There is grass! Trees with green leaves! Daylight until 1 am! And lots & lots of rain which produces copious amounts of mud. I forgot my umbrella, but I did arrive equipped with an insanely cheery pair of child-size "fireman style" rubber boots:
 I'm staying at one of the hospital-owned apartments next door to the jail (I will not lie--the barbed wire fence does give off penitentiary vibes). So far, the prisoners have been extremely quiet and neighborly. There is a super muddy trail leading from the apartments straight to the hospital that can be traversed in less than 5 minutes. It's hard to believe that I can squeeze through the narrow gap between two barbed wire fences--wearing all my waterproof gear and my internal frame pack--without setting off several alarms and alerting the Alaska State Troopers.
I'm staying at one of the hospital-owned apartments next door to the jail (I will not lie--the barbed wire fence does give off penitentiary vibes). So far, the prisoners have been extremely quiet and neighborly. There is a super muddy trail leading from the apartments straight to the hospital that can be traversed in less than 5 minutes. It's hard to believe that I can squeeze through the narrow gap between two barbed wire fences--wearing all my waterproof gear and my internal frame pack--without setting off several alarms and alerting the Alaska State Troopers.
Meanwhile, back on the inpatient wards, I feel like I'm swimming in jello, and everything I do is soooo slow and cumbersome. I have a large service of patients who have been here forever, many with tricky family dynamics that must be navigated carefully. The RMT calls are as crazy as I remembered, and today's top prize goes to a call about a 79-yr-old woman who had chest pain, then dramatically collapsed in the doorway of the village clinic, then went into bradycardia with a pulse of 40 followed by a seizure after receiving one dose of nitroglycerin. After being medevac'd to the ER, she was found to have a very low hemoglobin of 6! Oh Bethel, how I've missed you...

Meanwhile, back on the inpatient wards, I feel like I'm swimming in jello, and everything I do is soooo slow and cumbersome. I have a large service of patients who have been here forever, many with tricky family dynamics that must be navigated carefully. The RMT calls are as crazy as I remembered, and today's top prize goes to a call about a 79-yr-old woman who had chest pain, then dramatically collapsed in the doorway of the village clinic, then went into bradycardia with a pulse of 40 followed by a seizure after receiving one dose of nitroglycerin. After being medevac'd to the ER, she was found to have a very low hemoglobin of 6! Oh Bethel, how I've missed you...
Friday, June 24, 2011
How My Job Search Is Like An Episode of The Bachelorette
It really is, if you imagine each potential employer as one of the bachelors. Also imagine the physician recruiter as Chris Harrison, the host of the show who guides the bachelorette through her deliberations before each rose ceremony when she has to decide which bachelors to keep and which ones to send home. I interviewed with 2 urgent care clinics and 2 primary care clinics, with the following impressions:
Bachelor/employer #1: practical, down-to-earth, confident
Bachelor/employer #2: organized, detail-oriented
Bachelor/employer #3: alarmingly charming
Bachelor/employer #4: arrived 10 minutes after I had already checked in for my interview. Didn't really ask me any questions, just rambled on about random topics and how "nobody in this clinic ever works full-time [wink wink]". I began to wonder if bachelor #4 had been imbibing alcoholic refreshments.
In the end, I went with bachelor/employer #1, an urgent care clinic with 12-hour shifts. A 3-year contract was signed, just like in professional sports, with a start date in October. I expect to see my face on a box of Wheaties any day now...
Bachelor/employer #1: practical, down-to-earth, confident
Bachelor/employer #2: organized, detail-oriented
Bachelor/employer #3: alarmingly charming
Bachelor/employer #4: arrived 10 minutes after I had already checked in for my interview. Didn't really ask me any questions, just rambled on about random topics and how "nobody in this clinic ever works full-time [wink wink]". I began to wonder if bachelor #4 had been imbibing alcoholic refreshments.
In the end, I went with bachelor/employer #1, an urgent care clinic with 12-hour shifts. A 3-year contract was signed, just like in professional sports, with a start date in October. I expect to see my face on a box of Wheaties any day now...
Saturday, May 07, 2011
Disneyland for Procedure Junkies
A few weeks ago, I went to Charleston, SC for a refresher course on joint injections and management of fractures, sprains and dislocations. In a strange twist of fate, the woman sitting next to me was one of the doctors at the family medicine clinic in Bethel! (and she reports they were still, in mid-April, buried under snow & ice). We all loved the joint injection models (shoulder, wrist, knee, hip) with electronic needles that emitted a pleasant beep whenever we correctly entered the joint space. Winning! It was unadulterated fun spending hours fashioning custom splints and casts for the upper and lower extremities of our classmates. We even got to put someone in a football uniform (complete with helmet and enormous shoulder pads) to practice c-spine stabilization & log rolling of sports injuries on the field.
Charleston is a gorgeous city on a peninsula flanked by the Ashley River and the Cooper River, filled with historic buildings dating from the pre-Civil War era.
Charleston is also home to The Citadel, MUSC (the most expensive medical school in the country--and no, their stethoscopes aren't made of gold. I checked.) and Hyman's Seafood Deli where you can get the most amazing crabcakes. So delicious, you never want to leave. But leave I had to, because the tornadoes were a-comin'...
 |
| Cooper River |
 |
| Not a real squad car |
Charleston is also home to The Citadel, MUSC (the most expensive medical school in the country--and no, their stethoscopes aren't made of gold. I checked.) and Hyman's Seafood Deli where you can get the most amazing crabcakes. So delicious, you never want to leave. But leave I had to, because the tornadoes were a-comin'...
 |
| Best. Crabcake. Ever |
Thursday, April 07, 2011
Filing Taxes As An Independent Contractor vs Throwing Acid On My Eyeballs
They're both equally painful. Why does the IRS make everything so horrifyingly complicated? In order to complete the 1040, I have to fill out Schedule C (for profit or loss from business) and Schedule SE (to calculate self-employment tax), then start working on 1040-ES (for 2011 estimated tax) to figure out a quarterly payment schedule for taxes that don't get withheld from my locum tenens gigs while making random guesses regarding what my total income in 2011 might turn out to be [Dear IRS, Are you aware that I am not psychic].
Don't even get me started on what constitutes allowable deductions for business expenses! I have read countless IRS publications & instruction booklets and wandered through confusing and ridiculously unhelpful worksheets & flow charts, and I still can't tell if my calculations are correct. The instructions tell me to divide line 9 by line 15, then multiply by 0.0239, then spritz with aerosolized frankincense and bake the whole thing in a front-loading crucible gas kiln at cone 04 for 8 days while doing the hokey pokey. Am I a minister, member of a religious order, or Christian Science practitioner? Am I a farmer or fisherman? Really?! This information is somehow crucial to sorting out the jumble of paperwork?! Hire a tax professional, you say? Yes, I really should have done that months ago but you've probably deduced by now that I am the world champion procrastinator when it comes to paperwork involving taxes. The idea of working the counter at McDonald's is starting to sound inexplicably attractive...
Don't even get me started on what constitutes allowable deductions for business expenses! I have read countless IRS publications & instruction booklets and wandered through confusing and ridiculously unhelpful worksheets & flow charts, and I still can't tell if my calculations are correct. The instructions tell me to divide line 9 by line 15, then multiply by 0.0239, then spritz with aerosolized frankincense and bake the whole thing in a front-loading crucible gas kiln at cone 04 for 8 days while doing the hokey pokey. Am I a minister, member of a religious order, or Christian Science practitioner? Am I a farmer or fisherman? Really?! This information is somehow crucial to sorting out the jumble of paperwork?! Hire a tax professional, you say? Yes, I really should have done that months ago but you've probably deduced by now that I am the world champion procrastinator when it comes to paperwork involving taxes. The idea of working the counter at McDonald's is starting to sound inexplicably attractive...
Tuesday, April 05, 2011
Spring Has Sprung

Having returned to Seattle (after admitting my last patient on night float: a 14-yr-old girl who overdosed on tylenol and then had to endure lectures from both me and the ER doc on Why Acetaminophen Is Not Your Friend), I am delighted to find that everything from daffodils to cherry blossoms is now in full bloom, even if there is still more drizzle than sunshine. I am thankful to be walking on actual pavement instead of snow & ice, armed only with a light windbreaker.
My precocious 3-1/2 yr old nephew has advanced by leaps & bounds while I've been away, and he can now write most letters of the alphabet with minimal assistance. He wants to learn words, so I've been constructing small sentences for him to trace over with color pencils:
Tuesday, March 29, 2011
RMT Gone Wild
Another night of nearly nonstop RMT calls, which can be neatly summed up like one of those Chinese restaurant menus where you choose options from each of two columns...
Column A Column B
S/he was drinking and got hit on the head with a guitar
got shot with a BB pellet
S/he was on a snow got stabbed with a knife
machine/4-wheeler and fell down
started having seizures
S/he was playing got into a fight
with a BB gun and drank 3 bottles of R&R
got run over by a 4-wheeler
One man who was extremely intoxicated and combative got stabbed in the chest but would not allow the village health aide to apply pressure to the wound. Under normal circumstances, I would have activated the medevac, but this patient was belligerent and uncooperative and stated he would refuse to fly to Bethel; so I had the health aide monitor him in clinic. She called with frequent updates (vital signs, bleeding check), and each time, I could hear the patient yelling loudly in the background. Finally, the health aide had the VPO (village police officer) cart the patient off to jail because he was out of control. I figured if the patient was running around and throwing things in clinic, the likelihood of a pneumothorax, hemothorax or cardiac trauma from the stab wound was pretty low.
Column A Column B
S/he was drinking and got hit on the head with a guitar
got shot with a BB pellet
S/he was on a snow got stabbed with a knife
machine/4-wheeler and fell down
started having seizures
S/he was playing got into a fight
with a BB gun and drank 3 bottles of R&R
got run over by a 4-wheeler
One man who was extremely intoxicated and combative got stabbed in the chest but would not allow the village health aide to apply pressure to the wound. Under normal circumstances, I would have activated the medevac, but this patient was belligerent and uncooperative and stated he would refuse to fly to Bethel; so I had the health aide monitor him in clinic. She called with frequent updates (vital signs, bleeding check), and each time, I could hear the patient yelling loudly in the background. Finally, the health aide had the VPO (village police officer) cart the patient off to jail because he was out of control. I figured if the patient was running around and throwing things in clinic, the likelihood of a pneumothorax, hemothorax or cardiac trauma from the stab wound was pretty low.
Saturday, March 26, 2011
Cama-i
Cama-i means hello in Yup'ik.
The Cama-i Dance Festival occurs over a 3-day weekend each year in late March, drawing performance groups (showcasing mainly traditional Yup'ik and Inupiat story dances) from rural Alaska and other regions. It is an exceptionally well-attended event accompanied by a Native crafts festival featuring intricate beadwork and fur accoutrements. There was even the promise of Hmong lion dancers this year [which I did not see because it's really really hard to sit on bleachers in a crowded high school gymnasium for more than a few hours at a time...]
Thursday, March 24, 2011
Night Float
Major highlights from the previous night:
19:05 RMT call from a village health aide regarding a 37-yr-old female who had been drinking, then blacked out and had an unwitnessed fall onto an unknown object that left a puncture wound at the crown of her head. During the day, we would have just put the patient on a commercial flight to Bethel for further evaluation in the ER and a possible head CT, but at night the major mode of transportation is medevac which should only be activated when critical care is necessary. Pt was as lucid as one can be while intoxicated, no alarming neurologic deficits, but the health aide called to report that the puncture wound was actively bleeding. The photos she sent over telemed were a bit blurry and did not give any sense of the depth of the wound. How to manage this by telephone? I told her to put several layers of gauze on the wound, then wrap it as tightly as humanly possible with an ace bandage, then apply ice to the region of the wound. 20 minutes later she called to report that the bleeding had stopped and the patient was sobering up. Disaster averted.
20:53 I admit a 16-yr-old boy with suicidal ideation whose parents were involved in a tragic murder-suicide just a few months ago; he was the one who discovered their bodies and had to break the news to his younger sisters. Suicide has become such an alarmingly common problem in the Yukon-Kuskokwim Delta that several of the Iditarod competitors this year dedicated their race to suicide prevention.
21:30 A 16-yr-old primip in OB who had just given birth several hours ago after a 3-day induction for mild preeclampsia starts bleeding. We give her 1000 mcg of misoprostol and the bleeding ceases. Her post-delivery CBC shows a drop in hematocrit from 34 to 23.4.
22:44 I pick up several ER patients, one of which is a 13-month-old girl with a nasty-looking abscess on her R posterior thigh with a large area of surrounding cellulitis. Her mother seems unconcerned about the infection, and I am worried about mother's ability to administer daily medication and manage dressing changes, so I decide to hospitalize the girl and start her on IV antibiotics. After perusing her old chart, I discover that she has been hospitalized twice in the past 8 months for large MRSA abscesses with cellulitis, and that her mother has been investigated by the Office of Children's Services for suspected neglect.
00:13 The OB nurse pages me because the 16-yr-old primip produced another large gush of bright red blood. I medicate her with fentanyl & versed, then manually extract a large 200 cc blood clot from her uterus and order an additional CBC for morning.
02:22 More RMT calls about infants in respiratory distress, both of whom end up getting medevac'd.
03:10 More ER patients, mostly with viral respiratory infections that are stable for discharge. The ones who don't have family or friends in Bethel can stay in the hospital-owned hostel overnight and return in the afternoon for a recheck before flying home to their villages.
04:31 Several RMT calls about minor injuries from fisticuffs. The health aides aren't trained to do laceration repair, so they mainly irrigate the wounds and apply butterfly bandages to hold the wound edges together.
06:17 A 21-yr-old primip is admitted to L&D in active labor and quickly progresses to complete dilation. Instead of the usual stoic tolerance of labor, this primip yells, "That f*ing hurts!" every 10 seconds while pushing her baby out. Thankfully, it only takes 4 pushes to deliver her vigorous baby boy.
19:05 RMT call from a village health aide regarding a 37-yr-old female who had been drinking, then blacked out and had an unwitnessed fall onto an unknown object that left a puncture wound at the crown of her head. During the day, we would have just put the patient on a commercial flight to Bethel for further evaluation in the ER and a possible head CT, but at night the major mode of transportation is medevac which should only be activated when critical care is necessary. Pt was as lucid as one can be while intoxicated, no alarming neurologic deficits, but the health aide called to report that the puncture wound was actively bleeding. The photos she sent over telemed were a bit blurry and did not give any sense of the depth of the wound. How to manage this by telephone? I told her to put several layers of gauze on the wound, then wrap it as tightly as humanly possible with an ace bandage, then apply ice to the region of the wound. 20 minutes later she called to report that the bleeding had stopped and the patient was sobering up. Disaster averted.
20:53 I admit a 16-yr-old boy with suicidal ideation whose parents were involved in a tragic murder-suicide just a few months ago; he was the one who discovered their bodies and had to break the news to his younger sisters. Suicide has become such an alarmingly common problem in the Yukon-Kuskokwim Delta that several of the Iditarod competitors this year dedicated their race to suicide prevention.
21:30 A 16-yr-old primip in OB who had just given birth several hours ago after a 3-day induction for mild preeclampsia starts bleeding. We give her 1000 mcg of misoprostol and the bleeding ceases. Her post-delivery CBC shows a drop in hematocrit from 34 to 23.4.
22:44 I pick up several ER patients, one of which is a 13-month-old girl with a nasty-looking abscess on her R posterior thigh with a large area of surrounding cellulitis. Her mother seems unconcerned about the infection, and I am worried about mother's ability to administer daily medication and manage dressing changes, so I decide to hospitalize the girl and start her on IV antibiotics. After perusing her old chart, I discover that she has been hospitalized twice in the past 8 months for large MRSA abscesses with cellulitis, and that her mother has been investigated by the Office of Children's Services for suspected neglect.
00:13 The OB nurse pages me because the 16-yr-old primip produced another large gush of bright red blood. I medicate her with fentanyl & versed, then manually extract a large 200 cc blood clot from her uterus and order an additional CBC for morning.
02:22 More RMT calls about infants in respiratory distress, both of whom end up getting medevac'd.
03:10 More ER patients, mostly with viral respiratory infections that are stable for discharge. The ones who don't have family or friends in Bethel can stay in the hospital-owned hostel overnight and return in the afternoon for a recheck before flying home to their villages.
04:31 Several RMT calls about minor injuries from fisticuffs. The health aides aren't trained to do laceration repair, so they mainly irrigate the wounds and apply butterfly bandages to hold the wound edges together.
06:17 A 21-yr-old primip is admitted to L&D in active labor and quickly progresses to complete dilation. Instead of the usual stoic tolerance of labor, this primip yells, "That f*ing hurts!" every 10 seconds while pushing her baby out. Thankfully, it only takes 4 pushes to deliver her vigorous baby boy.
Tuesday, March 22, 2011
Breaking & Entering
From the Delta Discovery, a local newspaper serving Bethel and the villages of southwestern Alaska:
"Burglar Caught On Video, Befriends Guard Dog
An intruder broke into the Westlake Hangar at the Bethel Airport during the early morning hours between 4:30 am and 5:15 am, causing extensive damage to a window and a steel door. The thief stole 42 bottles of alcohol. The vandal used a sledgehammer. He also rifled through everything. The thief left behind 3 hammers."
"Burglar Caught On Video, Befriends Guard Dog
An intruder broke into the Westlake Hangar at the Bethel Airport during the early morning hours between 4:30 am and 5:15 am, causing extensive damage to a window and a steel door. The thief stole 42 bottles of alcohol. The vandal used a sledgehammer. He also rifled through everything. The thief left behind 3 hammers."
Sunday, March 20, 2011
Balmy, then...KABOOM!
For the past few days, it has been downright balmy, with temperatures in the mid-30s, ice melting, puddles forming on the side of the road. Last night brought the emergence of the Supermoon (the largest full moon since 1993!), as the moon arrived at its perigee, the point in its orbit closest to the earth.
All was well until the spring equinox today brought gale force winds and a snow storm. All flights between Bethel and the outlying villages have been canceled due to weather; even the medevac has been grounded. The RMT calls from the villages were pouring in nonstop:
-A 61-yr-old male with blood intermittently oozing out of his penis but no recent injury or trauma...the health aide estimated a half cup of blood had dribbled out within the past hour. I spoke with the on-call urologist in Anchorage who suggested attempting gentle insertion of a foley catheter for tamponade until the planes can bring the patient in for further evaluation. Apparently urethral injury is not a urologic emergency.
-A pregnant multip in active labor at 39 weeks who had missed her "Be in Bethel" date, baby delivered by the health aide who gave us a blow-by-blow account over the phone as it was happening.
-A 6-month-old baby in respiratory distress: tachypnea, hypoxia, tachycardia, fever of 100.7. The health aide was treating the baby with oxygen, albuterol nebulizer, and ceftriaxone IM and checking in with us every 2 hours while waiting for the weather to improve so medevac could resume flights.
As Aurelie has mentioned, if medevac is grounded, a Blackhawk helicopter can be summoned in life & death situations...and it's nerve-racking to be the one who determines what constitutes "life & death".
Meanwhile I was attempting a massive diuresis of my service before the next set of ward docs start tomorrow. My two loony-bin suicidal adolescent patients (one pregnant, the other withdrawing from an alcohol binge) on Title 47 (involuntary psychiatric hold for danger to self, danger to others, or grave disability) were awaiting transfer to the psychiatric facility in Anchorage. My intoxicated 49-yr-old female with fractured ribs and a tiny pneumothorax not apparent on chest x-ray, but seen on chest CT: when would it be safe for her to fly home to her village? I checked with the on-call pulmonologist in Anchorage who estimated 5 days after complete resolution of the pneumothorax. My patient can't get home without flying...unless she goes on a several-hours-long ride via snow machine over the bumpy frozen river, which would be quite painful with cracked ribs...
At the end of a very hectic day, I walked home from the hospital in the middle of a blizzard. At least all the waterproof gear I got at REI has proven to be truly waterproof.
All was well until the spring equinox today brought gale force winds and a snow storm. All flights between Bethel and the outlying villages have been canceled due to weather; even the medevac has been grounded. The RMT calls from the villages were pouring in nonstop:
-A 61-yr-old male with blood intermittently oozing out of his penis but no recent injury or trauma...the health aide estimated a half cup of blood had dribbled out within the past hour. I spoke with the on-call urologist in Anchorage who suggested attempting gentle insertion of a foley catheter for tamponade until the planes can bring the patient in for further evaluation. Apparently urethral injury is not a urologic emergency.
-A pregnant multip in active labor at 39 weeks who had missed her "Be in Bethel" date, baby delivered by the health aide who gave us a blow-by-blow account over the phone as it was happening.
-A 6-month-old baby in respiratory distress: tachypnea, hypoxia, tachycardia, fever of 100.7. The health aide was treating the baby with oxygen, albuterol nebulizer, and ceftriaxone IM and checking in with us every 2 hours while waiting for the weather to improve so medevac could resume flights.
As Aurelie has mentioned, if medevac is grounded, a Blackhawk helicopter can be summoned in life & death situations...and it's nerve-racking to be the one who determines what constitutes "life & death".
Meanwhile I was attempting a massive diuresis of my service before the next set of ward docs start tomorrow. My two loony-bin suicidal adolescent patients (one pregnant, the other withdrawing from an alcohol binge) on Title 47 (involuntary psychiatric hold for danger to self, danger to others, or grave disability) were awaiting transfer to the psychiatric facility in Anchorage. My intoxicated 49-yr-old female with fractured ribs and a tiny pneumothorax not apparent on chest x-ray, but seen on chest CT: when would it be safe for her to fly home to her village? I checked with the on-call pulmonologist in Anchorage who estimated 5 days after complete resolution of the pneumothorax. My patient can't get home without flying...unless she goes on a several-hours-long ride via snow machine over the bumpy frozen river, which would be quite painful with cracked ribs...
At the end of a very hectic day, I walked home from the hospital in the middle of a blizzard. At least all the waterproof gear I got at REI has proven to be truly waterproof.
Friday, March 18, 2011
A Word About Permafrost
 It's underground. It's composed of rocks, soil and frozen water. It forms when the depth of winter freezing exceeds the depth of summer thawing. If permafrost begins to melt, the ground above becomes waterlogged, soft, and prone to collapsing. Hence the proliferation of boardwalks & ramps in Bethel.
It's underground. It's composed of rocks, soil and frozen water. It forms when the depth of winter freezing exceeds the depth of summer thawing. If permafrost begins to melt, the ground above becomes waterlogged, soft, and prone to collapsing. Hence the proliferation of boardwalks & ramps in Bethel. To avoid melting the permafrost, the buildings in Bethel are built on stilts, and water & sewer pipes are installed above the ground.
Contact with the outside world? You can't get cell phone reception here unless you use a phone card or have an account with the local wireless company, but there is decent internet access and satellite television.
Wednesday, March 16, 2011
Overheard on Labor & Delivery
Here, in the land of pregnant ladies (both primips and multips alike) who are mysteriously able to deliver most of their babies in just 3 pushes, one of the OB nurses was musing over a non-native delivery she had just seen in which the expectant mother (loaded up on pitocin, with FSE & IUPC in place) had to push for 90 minutes before her baby emerged.
Nurse: (somewhat puzzled) I heard that's normal...
I confirmed that yes, in the lower 48 states, many primips do end up pushing for up to 2 hours. It really gives me pause about the medicalization of labor: in medical school & residency, most of the deliveries I saw involved breaking down the bed, feet placed in stirrups for pushing; intrauterine pressure catheters to measure the force of contractions; fetal scalp electrodes to better capture the fetal heart tracing; and of course IV pitocin for augmentation/induction of labor. Here in Bethel, the bed is often kept intact and instrumentation is kept to a minimum. Shorter 2nd stage of labor, cuter babies...
Nurse: (somewhat puzzled) I heard that's normal...
I confirmed that yes, in the lower 48 states, many primips do end up pushing for up to 2 hours. It really gives me pause about the medicalization of labor: in medical school & residency, most of the deliveries I saw involved breaking down the bed, feet placed in stirrups for pushing; intrauterine pressure catheters to measure the force of contractions; fetal scalp electrodes to better capture the fetal heart tracing; and of course IV pitocin for augmentation/induction of labor. Here in Bethel, the bed is often kept intact and instrumentation is kept to a minimum. Shorter 2nd stage of labor, cuter babies...
Tuesday, March 15, 2011
Qayagaluku

The difficulty of working on the wards is that your attention is pulled into 3 different directions:
1. Hospitalized patients (both adult and pediatric): the most prevalent reasons for admission on my service currently are multilobar pneumonia, frighteningly large & out-of-control abscesses, and alcohol withdrawal. There was a bit of drama today with a young lady brought in for suicidal ideation who turned out to have been diagnosed with TB one year ago and somehow successfully evaded treatment. Now she's captured in a negative-pressure isolation chamber, moody and crying, while Public Health tries to get a court order for her to remain in isolation until adequate treatment has begun.
Alcohol withdrawal came in the form of a married couple, both prone to DTs, sharing a room and a 24-hour sitter.
Day 1: Rowdy and drunk
Day 2: Still drunk
Day 3: Sleepy and drunk
2. OB patients: I delivered my first Native Alaskan baby a few days ago, an adorable rosy-cheeked infant who popped out after just 3 pushes. The L&D nurses here are refreshingly pleasant and extraordinarily helpful. And they gave me a salad! My first fresh veggies since arriving a week ago! I feel like my hospital-issue lime green scrubs are mocking the lack of fresh fruit in my diet:
3. RMT: a.k.a. Radio Medical Traffic, a term from the old days when communication was via two-way radio. In order to provide health care even in the most remote villages, each village has health aides who are on-call 24 hours. The health aides are equipped with a rudimentary clinic and modern technology that enables them to transmit digital images of patients and fax clinical notes to doctors at the hospital for feedback. I'm responsible for reviewing the notes & images from health aides, then calling them to discuss the patients. If you don't call them soon enough, they will hunt you down and have you paged repeatedly. In my head, I've been lumping the cases into 3 different categories: Benign (OK to treat in the village), Scary (take a commercial flight to Bethel for further evaluation!), and Scarier (medevac NOW!). Sometimes the health aides are frighteningly complacent.
Me: Is this 4-month-old baby really breathing 80 breaths per minute?
Health aide: (calmly) yes
Me: AAAAEEEEEEEEAAGGGGGHH! (translation: give her oxygen & a nebulizer treatment while I activate the medevac!)
Subscribe to:
Comments (Atom)

































