Thanks to freezing rain and the prospect of an ice storm, flight 42 to Anchorage has been canceled, so I am stranded in Bethel until tomorrow. To add insult to injury, I've developed a minor case of impetigo, a Staph infection most commonly seen in small children and wrestlers; luckily, I am paranoid enough to have brought Bactroban with me so I can slather my right philtrum with its strong antibacterial formula TID.
Thankfully, I also have the tendency to bring too much food with me on these excursions to rural southwest Alaska. This time, I cooked and froze lentil soup, chicken casserole, and runza (a Nebraskan treat made of ground beef, cabbage and onions with allspice & coriander, enveloped in a delicious homemade dough). The food gets transported efficiently in my checked baggage, and is usually still frozen by the time I land in Bethel, because the cargo hold on the plane is very chilly. I must confess I did eat runza for breakfast this morning (Beef! The breakfast of champions!). For the rest of the day, I will most likely imbibe hot tea, munch on popcorn, and watch 1000 consecutive episodes of "The West Wing" on DVD. Any television show or movie about medicine, hospitals or Alaska (or about practicing medicine in hospitals in Alaska) is strictly off-limits.
Mollusk
Home of the Sinister Bivalve
Tuesday, November 13, 2012
Monday, November 12, 2012
Where Are My Jelly Candies???!
Yes, this is what I've been reduced to: after 9 exhausting days on the inpatient wards and the possibility that my flight out of Bethel tomorrow may be cancelled due to freezing rain, all I can do is turn my room inside out in a herculean effort to locate the tiny prized bag of berry-shaped jelly candies with vitamin C that I got from the hospital vending machine in a feat of fortuitous timing. The vending machine can remain in a sad state of neglect and near-emptiness for quite a while before it gets re-stocked with snacks, and I was lucky enough to venture by just after a new supply was deployed. Combine that with my fear of scurvy, and you can see why I am so preoccupied...
My patient with endometritis & postpartum hemorrhage was discharged home today, freshly showered, hair in pigtails, looking much happier. Her first night here was a frightening one that involved being transferred from the floor to the ED (which functions as a pseudo ICU for patients who are too sick for the wards and are awaiting transport to a higher level of care in Anchorage), massive blood transfusion (5 units of pRBCs) and fluid resuscitation (5 liters of NS!). After a few days on a triple cocktail of clindamycin, gentamicin and ampicillin, she looks fantastic and no longer needs antibiotics.
Mr Lice Infestation left AMA this morning, but was willing to carry home several large bottles of permethrin for his wife and adult son to slather themselves in.
My 63-yr-old patient who was admitted for seizures after a 3-day drinking binge in which she completely abandoned her daily dose of keppra has finally started eating and looking a little more lucid. She was getting wheeled down the hallway as I left, and she gave me a perfect Queen Elizabeth coronation wave of her right hand, nodded her head, and gravely shook my hand, telling me "Quyana" which is Yup'ik for thank you.
My patient with endometritis & postpartum hemorrhage was discharged home today, freshly showered, hair in pigtails, looking much happier. Her first night here was a frightening one that involved being transferred from the floor to the ED (which functions as a pseudo ICU for patients who are too sick for the wards and are awaiting transport to a higher level of care in Anchorage), massive blood transfusion (5 units of pRBCs) and fluid resuscitation (5 liters of NS!). After a few days on a triple cocktail of clindamycin, gentamicin and ampicillin, she looks fantastic and no longer needs antibiotics.
Mr Lice Infestation left AMA this morning, but was willing to carry home several large bottles of permethrin for his wife and adult son to slather themselves in.
My 63-yr-old patient who was admitted for seizures after a 3-day drinking binge in which she completely abandoned her daily dose of keppra has finally started eating and looking a little more lucid. She was getting wheeled down the hallway as I left, and she gave me a perfect Queen Elizabeth coronation wave of her right hand, nodded her head, and gravely shook my hand, telling me "Quyana" which is Yup'ik for thank you.
Friday, November 09, 2012
Mucomyst for Dummies
Now we've got a strange combination of rain from the sky with stubbornly persistent slush and ice on the ground, and all flights have been cancelled. Medevac has been on hold for most of the day, so the RMT calls have been out of control. There are patients in the villages with broken ankles and dislocated shoulders who can't book a flight out because of the weather, and we can't activate a medevac for a non life-threatening condition. Some of the smaller clinics are running low on morphine and tylenol #3 for the patients with painful injuries who can't get to Bethel.
To top it off, I get 12 calls from a health aide about a 17-yr-old girl who was drinking last night and suspects she may have been sexually assaulted but can't recall the exact details. She started feeling depressed, so she decided to overdose on tylenol. She tells the health aide that she took 10 of the 325 mg tablets; when I briefly consult with the ER doc, he says there is no way to confirm whether the girl took 10 tablets or 100 tablets since depressed adolescents are notoriously unreliable historians, so she needs to take the oral mucomyst that is standard issue at all the village clinics, given the astoundingly high rate of suicide attempts here by tylenol overdose. The health aide tells me she can't find the mucomyst. I ask her if maybe someone else knows where it is. She calls me back to say no one can find any mucomyst anywhere. I ask her to check with Emmonak which is the nearest village. She calls me back to say that Emmonak has no mucomyst. After conferring with the ER doc again, we decide the girl needs to come in because excess tylenol could seriously fry her liver, so I activate the medevac. The health aide calls 10 minutes later to say actually Emmonak does have mucomyst and they will send it over. I call medevac and apologize profusely for wasting their time.
Meanwhile, between checking on my 82-yr-old patient admitted for an egregiously out-of-control lice infestation (I feel mildly pruritic just thinking about it) and chatting with a floridly psychotic 31-yr-old male on a psychiatric hold who wants to know if my pager is a recording device and whether I believe in human clones, I have sketched out a frighteningly detailed flow chart for the health aide who is waiting for the mucomyst to arrive because she seems a little...confused. Mucomyst for Dummies, based on the 17-yr-old girl's weight in kilograms, tracing out various dosing schemes depending on whether Emmonak sends the 10% or the 20% solution. Apparently mucomyst has an extraordinarily unpalatable flavor, so it needs to be mixed 1:3 with a deliciously cold beverage like orange juice or soda. Otherwise, no one would want to drink it. Frankly, I think their marketing department should consider changing the name of the product to something that sounds more...appetizing.
To top it off, I get 12 calls from a health aide about a 17-yr-old girl who was drinking last night and suspects she may have been sexually assaulted but can't recall the exact details. She started feeling depressed, so she decided to overdose on tylenol. She tells the health aide that she took 10 of the 325 mg tablets; when I briefly consult with the ER doc, he says there is no way to confirm whether the girl took 10 tablets or 100 tablets since depressed adolescents are notoriously unreliable historians, so she needs to take the oral mucomyst that is standard issue at all the village clinics, given the astoundingly high rate of suicide attempts here by tylenol overdose. The health aide tells me she can't find the mucomyst. I ask her if maybe someone else knows where it is. She calls me back to say no one can find any mucomyst anywhere. I ask her to check with Emmonak which is the nearest village. She calls me back to say that Emmonak has no mucomyst. After conferring with the ER doc again, we decide the girl needs to come in because excess tylenol could seriously fry her liver, so I activate the medevac. The health aide calls 10 minutes later to say actually Emmonak does have mucomyst and they will send it over. I call medevac and apologize profusely for wasting their time.
Meanwhile, between checking on my 82-yr-old patient admitted for an egregiously out-of-control lice infestation (I feel mildly pruritic just thinking about it) and chatting with a floridly psychotic 31-yr-old male on a psychiatric hold who wants to know if my pager is a recording device and whether I believe in human clones, I have sketched out a frighteningly detailed flow chart for the health aide who is waiting for the mucomyst to arrive because she seems a little...confused. Mucomyst for Dummies, based on the 17-yr-old girl's weight in kilograms, tracing out various dosing schemes depending on whether Emmonak sends the 10% or the 20% solution. Apparently mucomyst has an extraordinarily unpalatable flavor, so it needs to be mixed 1:3 with a deliciously cold beverage like orange juice or soda. Otherwise, no one would want to drink it. Frankly, I think their marketing department should consider changing the name of the product to something that sounds more...appetizing.
Thursday, November 08, 2012
Flakes of Snow
The inpatient wing recently got a makeover with mesmerizingly gorgeous simulated wood laminate flooring that makes it look like a spa. Very soothing to look at in the midst of complete chaos. Upon arrival to the hospital this morning, I was given a heads up from the night float about a patient arriving via medevac who had given birth to a stillborn infant at 29 + 5/7 wks EGA, had retained placenta for more than 3 hours, and was being transfused in transit with 2 units of blood for postpartum hemorrhage. By the time the patient arrived, I had already discharged 4 patients and admitted 2 new ones. She was strapped to a gurney, very quiet, with part of a placenta (clamped umbilical cord still attached) protruding slightly from her vagina, actively bleeding. The paramedics had given her almost 5L of IVF and her SBP was only in the high 80s to low 90s.
After drawing blood for CBC, type & cross, and bile acids (cholestasis of pregnancy is a common cause of fetal demise here), the OB nurses started infusing 20 units of pitocin. The placenta was manually extracted, and I did a quick repair of the patient's 1st degree vaginal laceration. Only after all the procedures were completed did the patient burst into tears. Admit her to OB or to the inpatient unit? The OB nurses were skilled with postpartum care, but it seemed insensitive to keep the patient where there were so many mothers with healthy newborns. The nurses pulled me into the supply area to assess the stillborn infant. He weighed just over 4 lbs and appeared to be at least 34 weeks old. They debated whether it would be all right to clean him up so the mother could have photographs taken; a quick call to the Medical Examiner (autopsy is mandatory in fetal demise beyond 20 weeks) confirmed that the stillborn infant had to be left in his current condition without any alteration.
The patient was transferred to the adult inpatient unit, doing well until she suddenly developed chills and tachycardia 20 minutes before the end of my shift. Minimal vaginal bleeding since the manual extraction of the placenta, no significant uterine tenderness, no dysuria or foul vaginal discharge. Pt's temperature skyrocketed from 97.6 to 101.8 within a matter of minutes. I got blood cultures, started clindamycin and gentamicin for presumed endometritis, and kept my fingers crossed.
Walking home, I noticed gentle flakes of snow falling from the sky and landing softly on the ground.
After drawing blood for CBC, type & cross, and bile acids (cholestasis of pregnancy is a common cause of fetal demise here), the OB nurses started infusing 20 units of pitocin. The placenta was manually extracted, and I did a quick repair of the patient's 1st degree vaginal laceration. Only after all the procedures were completed did the patient burst into tears. Admit her to OB or to the inpatient unit? The OB nurses were skilled with postpartum care, but it seemed insensitive to keep the patient where there were so many mothers with healthy newborns. The nurses pulled me into the supply area to assess the stillborn infant. He weighed just over 4 lbs and appeared to be at least 34 weeks old. They debated whether it would be all right to clean him up so the mother could have photographs taken; a quick call to the Medical Examiner (autopsy is mandatory in fetal demise beyond 20 weeks) confirmed that the stillborn infant had to be left in his current condition without any alteration.
The patient was transferred to the adult inpatient unit, doing well until she suddenly developed chills and tachycardia 20 minutes before the end of my shift. Minimal vaginal bleeding since the manual extraction of the placenta, no significant uterine tenderness, no dysuria or foul vaginal discharge. Pt's temperature skyrocketed from 97.6 to 101.8 within a matter of minutes. I got blood cultures, started clindamycin and gentamicin for presumed endometritis, and kept my fingers crossed.
Walking home, I noticed gentle flakes of snow falling from the sky and landing softly on the ground.
Wednesday, November 07, 2012
Dust Bowl of the North
Against my better judgement (what sane person would want to willingly trek northward to subzero temperatures?), I'm back in Bethel for another round of pummeling on the inpatient wards. There's something very endearing about the staff and the native Alaskan patients...or maybe I'm overconfident and delusional because I have a pair of ice cleats and a goosedown Goretex parka rated to -40 degrees, neither of which are needed at this moment because of the odd weather situation: daytime temperatures in the teens (but mildly subzero with the wind chill factor) and not a speck of snow on the ground.
The roads are hazardous to pedestrians when the climate is dry and windy; sidewalks are rare, and with every car that passes by, a giant cloud of dust swirls up to assault your eyes, nose and mouth. Luckily, I just had my annual respiratory fit test and my teal blue N95 respiratory mask matches my REI windbreaker. Making my twice daily trek between the residence and the hospital armed with the N95 mask and my headlamp, I look like a crazed (but stylish?) coal miner who is afraid of SARS.
Speaking of N95, I seem to be accumulating quite a few patients who require isolation rooms for a TB rule out. They're all awaiting results of sputum cultures for acid-fast bacilli. One patient was admitted for hip pain after being hit by a van and had a RLL cavitary lesion found incidentally on CT. Another was admitted for pneumonia with slightly blood-tinged sputum and mentioned being in contact with someone with active TB a few months ago. The third patient told the nurse she coughed up blood, then later back-pedaled and said the blood came from her nose. Too late, you win an instant PPD placement and a couple of days in isolation, booyah!
The roads are hazardous to pedestrians when the climate is dry and windy; sidewalks are rare, and with every car that passes by, a giant cloud of dust swirls up to assault your eyes, nose and mouth. Luckily, I just had my annual respiratory fit test and my teal blue N95 respiratory mask matches my REI windbreaker. Making my twice daily trek between the residence and the hospital armed with the N95 mask and my headlamp, I look like a crazed (but stylish?) coal miner who is afraid of SARS.
Speaking of N95, I seem to be accumulating quite a few patients who require isolation rooms for a TB rule out. They're all awaiting results of sputum cultures for acid-fast bacilli. One patient was admitted for hip pain after being hit by a van and had a RLL cavitary lesion found incidentally on CT. Another was admitted for pneumonia with slightly blood-tinged sputum and mentioned being in contact with someone with active TB a few months ago. The third patient told the nurse she coughed up blood, then later back-pedaled and said the blood came from her nose. Too late, you win an instant PPD placement and a couple of days in isolation, booyah!
Monday, September 17, 2012
Abdominal X-Ray, Anyone?
For most patients who come in for evaluation of abdominal pain, an x-ray rarely elucidates the etiology of the pain, with a couple of rare exceptions:
1. An 18-yr-old male accompanied by his mother is here for a one week history of vague symptoms: intermittent nausea and vomiting, generalized achy abdominal pain, no fever. It was difficult to get much detail from the patient, who was quite taciturn. [A preceptor that I worked with in medical school would often compare trying to elicit information from sullen adolescents to "veterinary medicine"]. The physical exam was not particularly remarkable; there was no abdomen rigidity or rebound tenderness. Imagine my surprise when the abdominal x-ray revealed a developing small bowel obstruction with air-fluid levels. Why would a previously healthy teenager with no surgical history develop SBO? Turns out he had a perforated appendicitis that was confirmed only by exploratory laparotomy.
2. A 38-yr-old man comes in for evaluation of sudden left-sided sharp abdominal pain that started at 4:00 am. I've learned to take it very seriously when people recall the exact time that a specific pain started. This man looked uncomfortable but was oddly dismissive of his pain, initially declining an abdominal x-ray. I am very glad that I finally talked him into it, because what showed up on the imaging was free air under the diaphragm which I had only read about but had never seen in real life. By this time, he had become tachycardic with a systolic blood pressure in the 80s, and he was promptly shipped off to the ED. The surgeon who took him to the OR found the source of the free air to be a perforated diverticulitis, remarking in the operative report: "This was the most pristine bowel I had ever seen". Five points to Gryffindor for having such a clean colon!
1. An 18-yr-old male accompanied by his mother is here for a one week history of vague symptoms: intermittent nausea and vomiting, generalized achy abdominal pain, no fever. It was difficult to get much detail from the patient, who was quite taciturn. [A preceptor that I worked with in medical school would often compare trying to elicit information from sullen adolescents to "veterinary medicine"]. The physical exam was not particularly remarkable; there was no abdomen rigidity or rebound tenderness. Imagine my surprise when the abdominal x-ray revealed a developing small bowel obstruction with air-fluid levels. Why would a previously healthy teenager with no surgical history develop SBO? Turns out he had a perforated appendicitis that was confirmed only by exploratory laparotomy.
2. A 38-yr-old man comes in for evaluation of sudden left-sided sharp abdominal pain that started at 4:00 am. I've learned to take it very seriously when people recall the exact time that a specific pain started. This man looked uncomfortable but was oddly dismissive of his pain, initially declining an abdominal x-ray. I am very glad that I finally talked him into it, because what showed up on the imaging was free air under the diaphragm which I had only read about but had never seen in real life. By this time, he had become tachycardic with a systolic blood pressure in the 80s, and he was promptly shipped off to the ED. The surgeon who took him to the OR found the source of the free air to be a perforated diverticulitis, remarking in the operative report: "This was the most pristine bowel I had ever seen". Five points to Gryffindor for having such a clean colon!
Thursday, August 09, 2012
The Natural History of Gel Shellac
I had my very first manicure done in preparation for a friend's wedding, and I foolishly allowed the manicurist to talk me into getting gel shellac applied to my fingernails. I am not particularly girly, and I rarely wear nail polish, so I am at a complete loss to explain what on earth possessed me to agree to a nail embellishment that would last for 3 weeks. The manicurist failed to mention that gel shellac can only be removed by either:
A. industrial strength solvent (100% acetone, which--if I recall correctly from a couple of organic chemistry labs that I survived eons ago--has potential toxic effects on the skin, reproductive system, and central nervous system), or
B. sanding with a power tool (I'm guessing some type of ladylike Martha Stewart style Dremel rotary tool)
Week 1
See how shiny and delightfully perky it looks initially? Gel shellac is baked on in several layers with the use of a special UV lamp, and it is designed to give you a manicure that won't chip or scratch during its entire 3 week tenure on your fingernails. But what if your nails grow at a freakishly rapid rate and you really don't feel like going to a nail salon to have the gel shellac removed by either method A or B?
Week 2
By the second week, I've already experienced a brisk fingernail growth spurt that exposes the nail base. But I will admit that the gel shellac still looks quite well preserved.
Week 4
Now you can really see the difference between the shiny gel shellac surface and the matte fingernail surface underneath...I start to develop a subconscious nervous habit of picking at the edges of the remaining gel shellac. I've noticed that the shellac softens a little after a hot shower, making it easier to peel away in small bits.
Week 5
Hooray, my thumbnails are free at last! I've still got gel shellac remnants on the other fingernails, and although I'm quite certain I look like a psychiatric inmate with too much time on my hands, I am fairly confident that I can peel away the rest of the gel shellac by the end of the week.
A. industrial strength solvent (100% acetone, which--if I recall correctly from a couple of organic chemistry labs that I survived eons ago--has potential toxic effects on the skin, reproductive system, and central nervous system), or
B. sanding with a power tool (I'm guessing some type of ladylike Martha Stewart style Dremel rotary tool)
Week 1
See how shiny and delightfully perky it looks initially? Gel shellac is baked on in several layers with the use of a special UV lamp, and it is designed to give you a manicure that won't chip or scratch during its entire 3 week tenure on your fingernails. But what if your nails grow at a freakishly rapid rate and you really don't feel like going to a nail salon to have the gel shellac removed by either method A or B?
Week 2
By the second week, I've already experienced a brisk fingernail growth spurt that exposes the nail base. But I will admit that the gel shellac still looks quite well preserved.
Week 4
Now you can really see the difference between the shiny gel shellac surface and the matte fingernail surface underneath...I start to develop a subconscious nervous habit of picking at the edges of the remaining gel shellac. I've noticed that the shellac softens a little after a hot shower, making it easier to peel away in small bits.
Week 5
Hooray, my thumbnails are free at last! I've still got gel shellac remnants on the other fingernails, and although I'm quite certain I look like a psychiatric inmate with too much time on my hands, I am fairly confident that I can peel away the rest of the gel shellac by the end of the week.
Thursday, July 19, 2012
Not Your Garden Variety Urgent Care Patients
Patient #1
He's an 88-yr-old man brought in by his adult son. For the past 2 days, the patient has been feeling dizzy and, curiously, leaning to the left (physically, not politically). "I feel like I'm on a ship," he tells me, holding onto the wall as he ambulates. His neurological exam is completely normal, except that he really does lean extraordinarily to his left side, even while perched on the exam table. There is no facial asymmetry, no hemiparesis, no aphasia, no slurred speech, no visual impairment. I send him to the ER because I'm worried he has had a stroke. His head CT was normal, but sure enough his MRI revealed evidence of a stroke in the posterior cerebellum.
Patient #2
A 76-yr-old man comes in and tells me his heart rate has been in the 30s for the past 4 days. He generally feels fine, although occasionally he experiences mild transient shortness of breath. An ECG reveals bradycardia at 35 bpm with complete atrioventricular block. I explain to him that his heart is beating very slowly because the upper portion of his heart is not communicating well with the lower portion of his heart. Although he looks remarkably well, he will probably need a pacemaker. He waves goodbye to me as the paramedics wheel him out on a gurney, smiling and winking as he clutches the Mario Puzo novel he's been reading. He gets a pacemaker inserted within hours of arriving in the ED.
Patient #3
A 53-yr-old man accompanied by his wife is here for what he calls a rash. "I thought it was an allergic reaction to something, " he says, and his wife adds, "We've been putting warm compresses on it and hoping it would go away." The left side of his face from his forehead to his cheek is remarkably red and swollen, and multiple pustules with yellowish discharge are visible. His left upper eyelid is so swollen he can barely open his eye which is exuding an endless stream of pus. His left sclera is erythematous, he has pain with eye movements, and there is slight proptosis. I sent him to the ER out of concern for herpes zoster ophthalmicus vs orbital cellulitis. On CT, an "incidental" brain tumor was found--and by incidental, they meant a 7.8 cm meningioma which had been miraculously asymptomatic. The patient got IV acyclovir, IV ceftriaxone, and a 12-hour craniotomy.
He's an 88-yr-old man brought in by his adult son. For the past 2 days, the patient has been feeling dizzy and, curiously, leaning to the left (physically, not politically). "I feel like I'm on a ship," he tells me, holding onto the wall as he ambulates. His neurological exam is completely normal, except that he really does lean extraordinarily to his left side, even while perched on the exam table. There is no facial asymmetry, no hemiparesis, no aphasia, no slurred speech, no visual impairment. I send him to the ER because I'm worried he has had a stroke. His head CT was normal, but sure enough his MRI revealed evidence of a stroke in the posterior cerebellum.
Patient #2
A 76-yr-old man comes in and tells me his heart rate has been in the 30s for the past 4 days. He generally feels fine, although occasionally he experiences mild transient shortness of breath. An ECG reveals bradycardia at 35 bpm with complete atrioventricular block. I explain to him that his heart is beating very slowly because the upper portion of his heart is not communicating well with the lower portion of his heart. Although he looks remarkably well, he will probably need a pacemaker. He waves goodbye to me as the paramedics wheel him out on a gurney, smiling and winking as he clutches the Mario Puzo novel he's been reading. He gets a pacemaker inserted within hours of arriving in the ED.
Patient #3
A 53-yr-old man accompanied by his wife is here for what he calls a rash. "I thought it was an allergic reaction to something, " he says, and his wife adds, "We've been putting warm compresses on it and hoping it would go away." The left side of his face from his forehead to his cheek is remarkably red and swollen, and multiple pustules with yellowish discharge are visible. His left upper eyelid is so swollen he can barely open his eye which is exuding an endless stream of pus. His left sclera is erythematous, he has pain with eye movements, and there is slight proptosis. I sent him to the ER out of concern for herpes zoster ophthalmicus vs orbital cellulitis. On CT, an "incidental" brain tumor was found--and by incidental, they meant a 7.8 cm meningioma which had been miraculously asymptomatic. The patient got IV acyclovir, IV ceftriaxone, and a 12-hour craniotomy.
Thursday, June 21, 2012
Vaginal Discharge with Sore Throat and No Insurance
It's always a dilemma when we see patients with no health insurance who are paying out of pocket for everything: you want to provide high quality medical care, but you don't want the patient to end up shelling out $800 just for one visit with a few lab tests that may or may not yield a diagnosis. So for the 23-yr-old female with thick yellow vaginal discharge and a sore throat, I had to ask...
Me: Are you sexually active?
Patient: No
Me: Have you ever had intercourse?
Patient: Yes
Me: When was the last time?
Patient: Wednesday
Me: Have you & your partner been having oral sex?
Patient: No
Me: At any time, was there a penis in your mouth?
Patient: Yes
Me: When?
Patient: Wednesday
For the vaginal discharge, I ended up doing a wet mount and a cervical swab for GC/CT. I had to make a decision about the sore throat: if it was due to a sexually-transmitted infection, I would have to perform separate throat swabs for chlamydia and gonorrhea, and the patient was concerned about paying for multiple tests with her limited funds. If it was due to respiratory infection, I could just order a rapid strep test. Luckily, the patient did have a low grade temperature of 100.2 with swollen tonsils, so we got a strep test and...it was POSITIVE.
Me: Are you sexually active?
Patient: No
Me: Have you ever had intercourse?
Patient: Yes
Me: When was the last time?
Patient: Wednesday
Me: Have you & your partner been having oral sex?
Patient: No
Me: At any time, was there a penis in your mouth?
Patient: Yes
Me: When?
Patient: Wednesday
For the vaginal discharge, I ended up doing a wet mount and a cervical swab for GC/CT. I had to make a decision about the sore throat: if it was due to a sexually-transmitted infection, I would have to perform separate throat swabs for chlamydia and gonorrhea, and the patient was concerned about paying for multiple tests with her limited funds. If it was due to respiratory infection, I could just order a rapid strep test. Luckily, the patient did have a low grade temperature of 100.2 with swollen tonsils, so we got a strep test and...it was POSITIVE.
Monday, May 21, 2012
Injuries in the Era of Digital Technology
When I saw "wrist laceration" on the list of chief complaints for patients waiting to be seen, I couldn't help wondering if it was due to a suicide attempt, and I half-expected to find a somewhat depressed individual in the procedure room. Instead, I discovered a rather cheerful, bon vivant 19-yr-old male flanked by his equally cheerful parents. He had been in the woods with his friends, participating in a Bored Teenager pastime: hurling hatchets at trees with the intention of embedding the blade in the trunks. The patient's grip on his hatchet slipped, and the blade made a 3 cm laceration that was just millimeters away from his radial artery. "Are you sure I didn't nick the artery?" he asked. I assured him that if he had severed his radial artery, he would have been gushing blood like a Monty Python skit. I was able to irrigate the wound and suture everything back into place with 3-0 ethilon. His parents, ever the enthusiasts, took video footage of the entire procedure with their iPhones so he could post it on his Facebook page.
Sunday, April 15, 2012
Possibly the Most Useful Thing I've Done in the Past 3 Months...
She was unfailingly polite, despite her embarrassment, as she introduced herself, shook my hand, and explained her problem. She and her husband had gotten rather tipsy the night before, and despite an exhaustive search of their bedroom, neither of them could find the condom they had used. "I think it's stuck somewhere inside me," she said tearfully.
After gently reassuring the patient, I was able to visualize the condom immediately upon inserting the speculum, and I neatly retrieved it with a handy pair of ring forceps. I told my greatly relieved patient not to feel bad and recited a litany of other items I had successfully removed from other people's vaginas, including an old tampon (the patient had cut the string off a few days before and forgotten about it) and a make-up sponge (I was afraid to ask).
After gently reassuring the patient, I was able to visualize the condom immediately upon inserting the speculum, and I neatly retrieved it with a handy pair of ring forceps. I told my greatly relieved patient not to feel bad and recited a litany of other items I had successfully removed from other people's vaginas, including an old tampon (the patient had cut the string off a few days before and forgotten about it) and a make-up sponge (I was afraid to ask).
Saturday, January 14, 2012
TB Or Not TB
A 15-yr-old girl came to the ED after 9 days of fever, night sweats, and productive cough that did not improve with antibiotics. She had been very healthy with no significant illnesses, so we were all shocked to see her CXR which revealed an astounding plethora of tiny pulmonary nodules. A chest CT also showed multiple tiny pulmonary nodules, along with a 1 cm cavitary lesion, which the pulmonologist in Anchorage agreed was highly suspicious for miliary tuberculosis which is disseminated hematogenously. Other conditions on the differential diagnosis included collagen vascular disease and neoplasm. Per protocol, I alerted the authorities (in this case, Alaska State Public Health and the office of Infection Control at the hospital) and started our patient on the potent 4-drug tuberculosis regimen. Two days later, her PPD was looking extremely positive, with a raised erythematous induration of 25 mm.
Friday, January 13, 2012
Medevac Wars
The other doc on wards with me got a call about a 50-yr-old male with bright red hematemesis and a rapidly falling hematocrit in one of the northwestern villages, so he activated the medevac to pick up the patient and bring him to the hospital. Fifteen minutes later, he got a call from one of the northeastern villages about a 61-yr-old male on antiepileptic medication who had been in status epilepticus for 20 minutes. The health aide did not have any ativan or diazepam in the clinic. My colleague had to activate the medevac again--but there was only one plane, and the two villages were quite far from each other. He & the ED doc conferred about which patient should be picked up first. They decided the man with the GI bleed was more critical, and as they directed the medevac to head northwest first, I called some of the northeastern villages to ask if they had any ativan or diazepam that someone could transport by snow machine to the patient having nonstop seizures. An hour later, the patient did get some diazepam delivered from a nearby village, and he was going to be next in line for the medevac, but then another call came in about a 5-yr-old girl with no known seizure disorder also in status epilepticus. The decision was made to medevac the girl first--it turns out she had a serum sodium of 110 (!) and marked neurologic abnormalities, and she ended up being transferred to Anchorage.
Thursday, January 12, 2012
If Work Doesn't Kill Me, This Virus Might
It's -24 degrees (closer to -40 degrees with the wind chill factor) and my lungs are very unhappy. The walk between the hospital and my current habitat is getting more painful as frost develops on my eyelashes, and my face literally hurts from being pummeled by the gelid winter wind. Bottom line: I have a huge stockpile of cab vouchers and I'm not afraid to use them!
I definitely have some kind of viral respiratory infection which makes my crazy work day feel a bit surreal. You! I mutter to my airways. Don't you dare succumb to a bacterial infiltration! One of the nurses very kindly offers me a highly prized (and much appreciated) chocolate truffle from Dilettante which I eat immediately, along with zinc gluconate lozenges and a ridiculously high dose of vitamin C. I make several calls to the hospital in Anchorage and to the medevac team about an 85-yr-old man with severe dementia and a slow GI bleed who needs to be transferred to a higher level of care. I am glad that I document everything so well in my notes, because I can't remember a single thing I said to either Anchorage or Lifemed. One of the ED docs hijacks my patient's medevac flight for a police officer who accidently shot himself in the leg with his service revolver and shattered his own femur.
Now I'm discharging 5 patients in rapid succession (including the 400-lb woman with a COPD exacerbation who keeps making up reasons to ask for ativan and morphine but still manages to be quite endearing). But wait! Is the 4-yr-old with RLL pneumonia really ready to fly home? Why has his WBC increased to 22? Can I blame it on the prednisolone? Five minutes later, his CRP comes back as 10.39, which is much improved from the initial value of 23--hooray! I have managed to complete all the discharge summary dictations, pushing through my viral haze with herculean effort. But I immediately get hit with 2 direct admissions: a elderly man with pneumonia from Kusko Clinic, and a 42-yr-old male with a bad case of LLE cellulitis extending to his groin from Delta Clinic. Then there are multiple garbled RMT calls from the health aide in Kipnuk: something about a possible suicide in the village...there's a pool of blood on the floor of someone's home...but the health aide isn't allowed inside the house because the state troopers are investigating the scene. It took an accumulated 30 minutes of phone calls to garner those juicy bits of information.
Now I'm swabbing the posterior fornix of a 20-yr-old primip at 31 weeks with preterm contractions in order to get a fetal fibronectin test. Don't touch your vagina, I told her 24 hours ago. Don't put anything inside your vagina, including your boyfriend's penis. Her ultrasound yesterday revealed a closed cervix measuring 2.7 cm which was mildly reassuring, but we couldn't get the FFN at the time because she was a couple of hours post-coitus.
Three hours later, an alternate medevac arrives to transfer my GI bleed patient to Anchorage and I am greatly relieved, because his hematocrit has dropped 10 points in 2 days and he can't get an EGD or colonoscopy at our tiny hospital due to his multiple comorbities. Where is the fried dough that the inpatient clerk gave me, I wonder. Did I eat it in my feverish delirium without realizing it? Probably.
I definitely have some kind of viral respiratory infection which makes my crazy work day feel a bit surreal. You! I mutter to my airways. Don't you dare succumb to a bacterial infiltration! One of the nurses very kindly offers me a highly prized (and much appreciated) chocolate truffle from Dilettante which I eat immediately, along with zinc gluconate lozenges and a ridiculously high dose of vitamin C. I make several calls to the hospital in Anchorage and to the medevac team about an 85-yr-old man with severe dementia and a slow GI bleed who needs to be transferred to a higher level of care. I am glad that I document everything so well in my notes, because I can't remember a single thing I said to either Anchorage or Lifemed. One of the ED docs hijacks my patient's medevac flight for a police officer who accidently shot himself in the leg with his service revolver and shattered his own femur.
Now I'm discharging 5 patients in rapid succession (including the 400-lb woman with a COPD exacerbation who keeps making up reasons to ask for ativan and morphine but still manages to be quite endearing). But wait! Is the 4-yr-old with RLL pneumonia really ready to fly home? Why has his WBC increased to 22? Can I blame it on the prednisolone? Five minutes later, his CRP comes back as 10.39, which is much improved from the initial value of 23--hooray! I have managed to complete all the discharge summary dictations, pushing through my viral haze with herculean effort. But I immediately get hit with 2 direct admissions: a elderly man with pneumonia from Kusko Clinic, and a 42-yr-old male with a bad case of LLE cellulitis extending to his groin from Delta Clinic. Then there are multiple garbled RMT calls from the health aide in Kipnuk: something about a possible suicide in the village...there's a pool of blood on the floor of someone's home...but the health aide isn't allowed inside the house because the state troopers are investigating the scene. It took an accumulated 30 minutes of phone calls to garner those juicy bits of information.
Now I'm swabbing the posterior fornix of a 20-yr-old primip at 31 weeks with preterm contractions in order to get a fetal fibronectin test. Don't touch your vagina, I told her 24 hours ago. Don't put anything inside your vagina, including your boyfriend's penis. Her ultrasound yesterday revealed a closed cervix measuring 2.7 cm which was mildly reassuring, but we couldn't get the FFN at the time because she was a couple of hours post-coitus.
Three hours later, an alternate medevac arrives to transfer my GI bleed patient to Anchorage and I am greatly relieved, because his hematocrit has dropped 10 points in 2 days and he can't get an EGD or colonoscopy at our tiny hospital due to his multiple comorbities. Where is the fried dough that the inpatient clerk gave me, I wonder. Did I eat it in my feverish delirium without realizing it? Probably.
Wednesday, January 11, 2012
My Nemesis Dr Tran
There is locums hospitalist named Dr Tran whose visits to Bethel often precede mine by one week or less. This causes a great deal of confusion, as many village health aides and hospital staff that I speak with on the phone will address me as "Dr Tran" even after repeated corrections. Although I have only met Dr Tran once (for about 5 minutes in March 2011), one of the OB nurses often asks me, "How is your little friend?" [referring slyly to Dr Tran]. It's mildly amusing, but I would be lying if I deny that some tiny evil part of me is occasionally tempted to wreak havoc and embark on a minor crime spree under the guise of being Dr Tran. But only while I'm in Bethel, of course.
Tuesday, January 10, 2012
You Know You've Been Thoroughly Bethel-ized When...
...you're excited to purchase your very first pair of ice cleats! Which, it turns out, I didn't really need because we're in the middle of a blizzard and snow drifts are blowing everywhere. I was completely blinded by the flurries furiously pounding my face and couldn't find the trail leading from the boardwalk to the hospital this morning; consequently, I found myself frequently stepping into knee-deep snow (2 thumbs up for my excellent ski pants, by the way, which marvelously kept snow out of my insulated boots!). All flights were canceled today--yes, even the 737 planes that fly between Bethel and Anchorage! Fortunately, the medevac is still running, and when I left the hospital tonight, they were duking it out over which kid in respiratory distress to pick up first (Emmonak vs Mekoryuk: discuss).
I was hoping to sample some elk stew or a reindeer burger during this week on the wards, but, alas the cafeteria has been serving mainly fried chicken, pork tenderloin, and tacos. My favorite patients are two frail elderly ladies (one who wears her hair in pigtails), both with hyponatremia and sharing the same hospital room. I finally got their serum sodium levels back to normal (one with a slow infusion of normal saline, the other with free water restriction) but now the one in pigtails is persistently dizzy, so I started her on a baby dose of meclizine. In other news, the hospital is still using paper charts, but there are intriguing rumors of an EMR launch scheduled for January 2013...
I was hoping to sample some elk stew or a reindeer burger during this week on the wards, but, alas the cafeteria has been serving mainly fried chicken, pork tenderloin, and tacos. My favorite patients are two frail elderly ladies (one who wears her hair in pigtails), both with hyponatremia and sharing the same hospital room. I finally got their serum sodium levels back to normal (one with a slow infusion of normal saline, the other with free water restriction) but now the one in pigtails is persistently dizzy, so I started her on a baby dose of meclizine. In other news, the hospital is still using paper charts, but there are intriguing rumors of an EMR launch scheduled for January 2013...
Monday, January 02, 2012
Mormon Fisticuffs and Other Sources of Excitement
New Year's eve was a wildly eventful day in clinic. From a 36-yr-old woman with probable pneumonia who was tachypneic and only satting 65% on room air but didn't want us to call an ambulance to transport her to the ED... to a tall 24-yr-old man with excellent cheekbones and a tiny laceration on his face requesting "just one stitch" and lamenting that the scar would ruin his not-yet-launched "modeling career"... to the most fresh-faced wholesome-looking 19-yr-old blond teenager in a dress shirt and pressed trousers sporting a swollen black eye and a scalp abrasion after getting in a fist fight with another church member at a Mormon holiday event...
We thought all the excitement was over after we finally finished treating the last patient about an hour after clinic was officially closed...but when I arrived back at work on New Year's day, there was a huge gaping hole in the northwestern corner of the clinic building, cordoned off with caution tape. Turns out a very inebriated driver from the nearby air force base collided into the clinic late at night, completely totaling his car...then he got up and walked over to Taco Bell (where he was arrested) because he suddenly felt extremely hungry.
We thought all the excitement was over after we finally finished treating the last patient about an hour after clinic was officially closed...but when I arrived back at work on New Year's day, there was a huge gaping hole in the northwestern corner of the clinic building, cordoned off with caution tape. Turns out a very inebriated driver from the nearby air force base collided into the clinic late at night, completely totaling his car...then he got up and walked over to Taco Bell (where he was arrested) because he suddenly felt extremely hungry.
Thursday, December 08, 2011
It's Official: Psychiatric Patients Are Really Liking My Hair Today
For the past 25 years, I've been secretly cutting my own hair. It started when I was in college and I had super thick waist-length hair. I initially intended to just give myself a slight trim, maybe an inch or two at the very most...but the smooth snip-snip of the scissors was ever so much fun! and addictive! It was really quite difficult to let go of the scissors, and 20 minutes later, I found myself sporting a jaunty chin-length bob.
I used to set up 2 mirrors--one in front of me, and one behind me--so that I could get a good view of the back of my head while trimming my hair. These days, I just use one mirror and I judge whether I'm cutting well by feeling the back of my head for uneven hair distribution. I snipped away at my hair last night, and for some bizarre reason, all of my clinic patients with psychiatric diagnoses have been complimenting my haircut today. Bipolar disorder with low back pain thought the shape framed my face nicely. Obsessive compulsive disorder with a sinus infection especially liked the way my bangs swayed liltingly to one side. Even the strange lady with panic disorder who was standing in the corner of the exam room crying and holding her left arm as if she were a bird with a broken wing told me my hair looked great. None of these patients had a primary care provider they could see for follow up.
I grew up in an era when everyone had a family doctor, and it is a constant puzzle to me when I see so many patients at our urgent care clinic who don't have a primary care provider but want to be treated for a chronic condition. Many patients feel they're "too healthy" to have a regular doctor; others complain about how long it takes to set up an appointment to establish care. I have encountered multiple patients with severe abdominal pain or pelvic pain who went to the ED and waited for a few hours while labs were drawn, then left the ED to seek medical attention at our urgent care clinic because they "got tired of waiting". Even though they were having excruciating pain and they could have had access to CT scans, MRIs, ultrasounds and stat lab results in the ED (none of which are available in urgent care), they left because they wanted to be seen "right away". Then they get upset when we direct them back to the ED because we can't provide the higher level of care that they need. Our healthcare system is broken, and none of it makes any sense, but at least the psychiatric patients really like my hair...
I used to set up 2 mirrors--one in front of me, and one behind me--so that I could get a good view of the back of my head while trimming my hair. These days, I just use one mirror and I judge whether I'm cutting well by feeling the back of my head for uneven hair distribution. I snipped away at my hair last night, and for some bizarre reason, all of my clinic patients with psychiatric diagnoses have been complimenting my haircut today. Bipolar disorder with low back pain thought the shape framed my face nicely. Obsessive compulsive disorder with a sinus infection especially liked the way my bangs swayed liltingly to one side. Even the strange lady with panic disorder who was standing in the corner of the exam room crying and holding her left arm as if she were a bird with a broken wing told me my hair looked great. None of these patients had a primary care provider they could see for follow up.
I grew up in an era when everyone had a family doctor, and it is a constant puzzle to me when I see so many patients at our urgent care clinic who don't have a primary care provider but want to be treated for a chronic condition. Many patients feel they're "too healthy" to have a regular doctor; others complain about how long it takes to set up an appointment to establish care. I have encountered multiple patients with severe abdominal pain or pelvic pain who went to the ED and waited for a few hours while labs were drawn, then left the ED to seek medical attention at our urgent care clinic because they "got tired of waiting". Even though they were having excruciating pain and they could have had access to CT scans, MRIs, ultrasounds and stat lab results in the ED (none of which are available in urgent care), they left because they wanted to be seen "right away". Then they get upset when we direct them back to the ED because we can't provide the higher level of care that they need. Our healthcare system is broken, and none of it makes any sense, but at least the psychiatric patients really like my hair...
Wednesday, November 16, 2011
85 Patients!!!
Most of the time, I enjoy my new job, but every now and then I have a truly horrifying day that takes the wind out of my sails. On Monday, I arrived at the clinic to find that I had been completely and inexplicably locked out of the computer network. While hordes of patients were piling up in the waiting room, I was on the phone with IT, desperately trying to log on to the network and then to the EMR. When I finally regained access to the EMR, I discovered that I could only log on using one specific computer and that I was mysteriously locked out of the computers in all of the exam rooms.
Much of the day went like this: 5 upper respiratory infections, low back pain, the EMR sends error messages telling me my password is invalid, I spend 20 minutes on the phone with IT trying to regain access to the EMR, I see 5 more upper respiratory infections, shoulder pain, 4 bladder infections, and I'm locked out of the EMR again, I spend 20 minutes on the phone with IT....lather, rinse, repeat.
By 8:30 pm, we had so many patients camped out in the waiting room, we had to divert some of them to a different urgent care clinic. It wasn't until 9:15 pm when the last patient left that I realized, in a sort of post-traumatic haze, that we had seen 85 patients. You heard me: 2 clinicians, 85 patients!
It wasn't all bad. There were certainly small triumphs, like removing a pedunculated growth (probably a small hemangioma) from a 14-yr-old's scalp--it had been present since birth, and the surrounding skin had gotten infected with impetigo, and it was such fun to watch her marvel over the newly smooth texture of her scalp after the procedure.
When I was in medical school, I developed coping mechanisms for stressful days on my 3rd and 4th year clinical rotations: my official theme song was Dean Martin's "Ain't That a Kick in the Head". On my PDA, I had video clips of my friends & family saying silly things like "I'll see you in hell!" and "I'd like to order a CBC, a BMP, and a glass of red wine" which would inevitably make me smile, even on bad call nights.
My coping mechanisms this winter are as follows: I've fashioned a tiny bracelet from 1/4" white elastic and, using iron-on transfer paper, decorated it with the phrase "Mischief managed!" which is what Harry Potter utters when he wants to close up the Marauder's Map at Hogwarts. It reminds me that, no matter how crazy my work day is, it does eventually come to an end. I've also been watching episodes of "Make It or Break It", an ABC Family drama about teenage girls who are elite gymnasts striving to make it to the 2012 Olympics. What I love about women's gymnastics is how the athletes get a big hug every time they complete a performance on the vault, the balance beam or the uneven bars. When I'm dreading the long commute to work, I imagine myself as a gymnastics girl in a shiny leotard, with glittery eye shadow and a fluffy hair scrunchy, with my coach and teammates yelling, "You can do it!", "You've got this!" and "Stick that landing!" from the sidelines. Silly, I know, but it does make me feel better.
Much of the day went like this: 5 upper respiratory infections, low back pain, the EMR sends error messages telling me my password is invalid, I spend 20 minutes on the phone with IT trying to regain access to the EMR, I see 5 more upper respiratory infections, shoulder pain, 4 bladder infections, and I'm locked out of the EMR again, I spend 20 minutes on the phone with IT....lather, rinse, repeat.
By 8:30 pm, we had so many patients camped out in the waiting room, we had to divert some of them to a different urgent care clinic. It wasn't until 9:15 pm when the last patient left that I realized, in a sort of post-traumatic haze, that we had seen 85 patients. You heard me: 2 clinicians, 85 patients!
It wasn't all bad. There were certainly small triumphs, like removing a pedunculated growth (probably a small hemangioma) from a 14-yr-old's scalp--it had been present since birth, and the surrounding skin had gotten infected with impetigo, and it was such fun to watch her marvel over the newly smooth texture of her scalp after the procedure.
When I was in medical school, I developed coping mechanisms for stressful days on my 3rd and 4th year clinical rotations: my official theme song was Dean Martin's "Ain't That a Kick in the Head". On my PDA, I had video clips of my friends & family saying silly things like "I'll see you in hell!" and "I'd like to order a CBC, a BMP, and a glass of red wine" which would inevitably make me smile, even on bad call nights.
My coping mechanisms this winter are as follows: I've fashioned a tiny bracelet from 1/4" white elastic and, using iron-on transfer paper, decorated it with the phrase "Mischief managed!" which is what Harry Potter utters when he wants to close up the Marauder's Map at Hogwarts. It reminds me that, no matter how crazy my work day is, it does eventually come to an end. I've also been watching episodes of "Make It or Break It", an ABC Family drama about teenage girls who are elite gymnasts striving to make it to the 2012 Olympics. What I love about women's gymnastics is how the athletes get a big hug every time they complete a performance on the vault, the balance beam or the uneven bars. When I'm dreading the long commute to work, I imagine myself as a gymnastics girl in a shiny leotard, with glittery eye shadow and a fluffy hair scrunchy, with my coach and teammates yelling, "You can do it!", "You've got this!" and "Stick that landing!" from the sidelines. Silly, I know, but it does make me feel better.
Thursday, November 10, 2011
Pattern Recognition
I recently saw a 36-yr-old female who had a 5-day history of vaginal irritation with a "burning" sensation. She was seen a few days earlier and given diflucan for a presumed yeast infection, but her condition had not improved. She told me, "It just really burns" and "When I try to pee, nothing comes out". Her UA and GC/CT were negative. On physical exam, her labia was erythematous and markedly swollen. I suddenly remembered the last time I saw a patient with a similarly swollen labia and the same complaint of dysuria and urinary retention: it was a 14-yr-old girl who had come to the pediatric ED where I was doing a residency rotation. We initially suspected cellulitis. She was in so much pain that conscious sedation was required for her pelvic exam. After a meticulous search, we finally found a vesicular lesion: it turned out this young girl had the worst case of genital herpes in the history of the universe.
I did manage to find one shallow ulcerated lesion on my 36-yr-old patient's perineum which I promptly swabbed for HSV culture. She was very skeptical about the provisional diagnosis of herpes, but she was willing to try taking acyclovir. A few days later, the culture came back positive for HSV-2.
I did manage to find one shallow ulcerated lesion on my 36-yr-old patient's perineum which I promptly swabbed for HSV culture. She was very skeptical about the provisional diagnosis of herpes, but she was willing to try taking acyclovir. A few days later, the culture came back positive for HSV-2.
Monday, October 31, 2011
Driving My Life Away
I'm very excited about finally starting my first permanent MD job. The lovely thing about urgent care is that patients generally present with just one or two medical problems. I will never complain about the following: lancing abscesses, suturing lacerations (I had to stitch across the vermilion border on a lip laceration recently!), removing a foreign body from someone's eye (the patient was a very skittish young man who kept twitching away from me and reflexively shutting his eyes, but I finally got the tiny brown speck after a saline eye wash and a few passes with a sterile cotton swab).
Aside from seeing multitudes of patients with viral respiratory infections who would have been better off staying home to rest, my only beef with this job is the commute: 55 minutes on I-5 to get to work, 55 minutes to get home. It would behoove me to invest in the Berlitz or Rosetta Stone Spanish language course on CD [conduzco mi vida lejos?] so I can learn while driving, and to start saving my pennies for a hybrid car, methinks.
Aside from seeing multitudes of patients with viral respiratory infections who would have been better off staying home to rest, my only beef with this job is the commute: 55 minutes on I-5 to get to work, 55 minutes to get home. It would behoove me to invest in the Berlitz or Rosetta Stone Spanish language course on CD [conduzco mi vida lejos?] so I can learn while driving, and to start saving my pennies for a hybrid car, methinks.
Friday, September 30, 2011
Hoh Hoh Hoh
The Hoh Rain Forest, which is part of the Olympic National Park, is truly a wonder of the Pacific Northwest. One of just a few temperate rain forests in the U.S., it encompasses 24 miles of low elevation forest along the Hoh River, and the average annual precipitation is an astonishing 12 to 14 feet of rain.
There are a couple of short trails that loop through the forest near the visitor's center (one of which was closed because the park rangers didn't want a family of Roosevelt elks to be disturbed), as well as the more hardcore 17 mile Hoh River Trail which leads to Glacier Meadows near Mount Olympus.
Maybe because of my lack of height, I find myself entranced by the intricate network of intertwined tree roots, especially evident in seedlings that begin their growth on top of fallen logs.
The high humidity, deep soil and mild temperatures contribute to the astounding size of the trees. I have the sneaking suspicion that if I fell down in the rain forest, moss would immediately start growing on me.
I would probably have to call for help from this phone booth...
There are a couple of short trails that loop through the forest near the visitor's center (one of which was closed because the park rangers didn't want a family of Roosevelt elks to be disturbed), as well as the more hardcore 17 mile Hoh River Trail which leads to Glacier Meadows near Mount Olympus.
Maybe because of my lack of height, I find myself entranced by the intricate network of intertwined tree roots, especially evident in seedlings that begin their growth on top of fallen logs.
The high humidity, deep soil and mild temperatures contribute to the astounding size of the trees. I have the sneaking suspicion that if I fell down in the rain forest, moss would immediately start growing on me.
I would probably have to call for help from this phone booth...
Thursday, September 22, 2011
Trying To Act Like A Professional
Imagine you're seeing a 58-yr-old patient in clinic for the first time who is having problems with chronic hip pain. He is very tan, and his weathered face slightly resembles Mel Brooks.
You are, of course, sympathetic to his pain, and you conduct a thorough exam which finds that his symptoms are consistent with a R hip bursitis with tenderness to palpation at the greater trochanter. You want to offer a steroid injection into the bursa for pain relief, but you are becoming increasingly more distracted by this patient's...hair.
He has amazingly shiny and very dark hair, styled in a manner that looks a bit like this wig, but in a much deeper shade of brown:
The distraction becomes overwhelming, and you step out of the room briefly, run into a colleague who looks at you quizzically, and, unable to suppress the inevitable burst of glee, you whisper furtively, "I've got a 58-yr-old male with Prince Valiant hair!"
You are, of course, sympathetic to his pain, and you conduct a thorough exam which finds that his symptoms are consistent with a R hip bursitis with tenderness to palpation at the greater trochanter. You want to offer a steroid injection into the bursa for pain relief, but you are becoming increasingly more distracted by this patient's...hair.
He has amazingly shiny and very dark hair, styled in a manner that looks a bit like this wig, but in a much deeper shade of brown:
The distraction becomes overwhelming, and you step out of the room briefly, run into a colleague who looks at you quizzically, and, unable to suppress the inevitable burst of glee, you whisper furtively, "I've got a 58-yr-old male with Prince Valiant hair!"
Saturday, September 17, 2011
Flattery Will Get You Everywhere
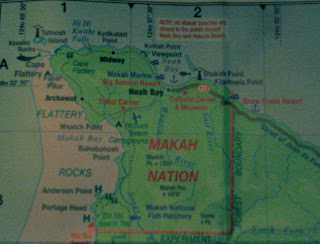
Cape Flattery is just 8 miles away, and it's known as the northwesternmost point of the contiguous United States. It was named in 1778 by British explorer Captain James Cook who noted from his ship, "there appeared to be a small opening which flattered us with the hopes of finding a harbour". The often muddy trail to the Cape is made less treacherous by strategic placement of cedar plank boardwalk constructed in 1996 by 7 members of the Makah tribe.
Once you get about halfway through the 3/4 mile trail, you start to hear the sound of the ocean, but you can't really tell where it's coming from until you approach the first observation deck.
There are 5 observation decks constructed with cedar planks and guard rails, with breathtaking views overlooking both the Pacific Ocean and the Strait of Juan de Fuca. You can see picturesque sea stacks with trees growing on top, sometimes populated by puffins. If you're lucky, you may catch otters sunning themselves on the rocks below.
Tatoosh Island, 1/2 mile off the coast from the Cape Flattery, is a former Makah fishing and whaling camp; the lighthouse on the island was built in 1857 and is owned & operated by the Coast Guard.
Once you get about halfway through the 3/4 mile trail, you start to hear the sound of the ocean, but you can't really tell where it's coming from until you approach the first observation deck.
There are 5 observation decks constructed with cedar planks and guard rails, with breathtaking views overlooking both the Pacific Ocean and the Strait of Juan de Fuca. You can see picturesque sea stacks with trees growing on top, sometimes populated by puffins. If you're lucky, you may catch otters sunning themselves on the rocks below.
Tatoosh Island, 1/2 mile off the coast from the Cape Flattery, is a former Makah fishing and whaling camp; the lighthouse on the island was built in 1857 and is owned & operated by the Coast Guard.
Also visible are a proliferation of sea caves which are dramatic openings worn into the cliffs by the constant pounding of the ocean waves. The entire experience of traveling through the forest, then suddenly being confronted by the stunning beauty of the coast is surprisingly emotional and awe-inspiring.
Friday, September 09, 2011
Blackberry Teeth and the Neah Bay Rumor Mill
Sometimes clinic staff will bring in a homemade treat to share with everyone. Today it was a beautiful and impressively large blackberry cobbler baked in a cast iron pan. Most of us managed to nibble on it intermittently throughout the morning, but it wasn't until 11:30 that the pharmacy assistant sidled up to me and whispered, "Everyone who ate the cobbler has blue teeth!" I surreptitiously glanced at my mouth in the nearest mirror, and lo & behold--my teeth had freakishly taken on the same shade as the blue sclera of osteogenesis imperfecta.
The nurse practitioner tells me that some of the older aunties of the town have been gossiping that Dr Chan "doesn't touch patients". I'm not sure what that means--could they be referring to my habit of donning latex gloves before coming into contact with bodily fluids (e.g. during a bimanual exam, while palpating a lesion on someone's buccal mucosa, or while lancing an abscess)?? Because that's called taking universal precautions. The lab tech joked that I should do trigger point injections by administering the lidocaine & kenalog via blowdart, instead of the usual syringe with 27-gauge needle, so I can continue "not touching patients".
The nurse practitioner tells me that some of the older aunties of the town have been gossiping that Dr Chan "doesn't touch patients". I'm not sure what that means--could they be referring to my habit of donning latex gloves before coming into contact with bodily fluids (e.g. during a bimanual exam, while palpating a lesion on someone's buccal mucosa, or while lancing an abscess)?? Because that's called taking universal precautions. The lab tech joked that I should do trigger point injections by administering the lidocaine & kenalog via blowdart, instead of the usual syringe with 27-gauge needle, so I can continue "not touching patients".
Tuesday, September 06, 2011
Escape to Victoria
I can't imagine what it's like to be one of only two full-time permanent doctors in a remote rural community, constantly being on call and rarely taking time off. One of the doctors has been here for 7 years, and he's familiar with all the idiosyncracies of our more--shall we say?--eccentric clinic patients; he's a proponent of kickin' it old school, meaning that he still spends the whole day in clinic after being on call the night before. He enjoys canning salmon by dividing the fish to fit half-pint mason jars to stew for 100 minutes in a pressure cooker. The result is surprisingly fresh and has a shelf life of two years. The other doctor is about a year out of residency (like me) with additional training in acupuncture and other types of alternative medicine, which is wonderful for the abundance of patients with chronic pain. So many people who work in the commercial fishing industry don't have time to drive 60 miles & back to see the nearest physical therapist, but they're willing to try a 15 to 20 minute session of acupuncture in the clinic.
Over Labor Day weekend, I drove to Port Angeles and hopped a ferry to Vancouver Island where I was absolutely delighted to eat gelato in a waffle cone (for breakfast!), catch an afternoon of the Vancouver Island Blues Bash, tour the Butchart Gardens, and just stroll around marveling at the architecture of the faintly Anglophilic city of Victoria, British Columbia.
Over Labor Day weekend, I drove to Port Angeles and hopped a ferry to Vancouver Island where I was absolutely delighted to eat gelato in a waffle cone (for breakfast!), catch an afternoon of the Vancouver Island Blues Bash, tour the Butchart Gardens, and just stroll around marveling at the architecture of the faintly Anglophilic city of Victoria, British Columbia.
 |
| The Empress Fairmont, where High Tea is served |
 |
| The Legislative Building, where the government lives |
 |
| The Japanese Garden at Butchart Gardens |
Saturday, August 27, 2011
These Boots Were Made For Walk-Ins
The clinic has 6 exam rooms and 1 small trauma room which is often used for minor accidents, since the closest hospital is 60 miles away in Forks (the land of Twilight aficionados). Most of the visits are walk-ins, and after a while it all blurs together at a very brisk pace: from the woman who marched into the waiting room demanding "PowerPoint injections" for bilateral elbow pain (I'll call Microsoft, stat! I thought to myself) to the young man who sheepishly admitted his chief complaint wasn't coughing, as he told the nurse, but actually a 3-day history of green penile discharge (Condoms! I croaked, while injecting him with ceftriaxone and making him swallow 1 gram of azithromycin)...at the end of the day, I'm usually dazed and hypoglycemic--that is, if I'm not too busy cursing the cumbersome Cro-Magnon era EMR.
I had the opportunity to use the trauma room yesterday when we received a radio report about a grass fire, which turned out to be a man on the grass who was on fire. The town was hit with an influx of visitors for the Makah Days Festival, a celebration of Makah culture involving canoe races, traditional dancing, vendors, a talent show, and a salmon bake. In the midst of all the excitement, a large barrel of heated roofing tar spontaneously combusted, and the patient sustained 2nd degree burns on his R hand and R leg. The EMTs brought him in on high-flow oxygen with a nonrebreather mask, already hooked up by IV to a 1-liter bag of normal saline. Although his nasal mucosa was mildly singed, he was breathing normally with no signs of airway edema. The blisters on his skin were starting to pop, and we debrided quite a bit of the dead skin from the burns.
After all the drama, I was able to slip away quietly this morning to meet up with my brother & his family who were camping 54 miles away at the Olympic National Park. We took a trip to La Push to spend the day at Rialto Beach which has a wildly beautiful rocky shoreline punctuated with silvery driftwood that has been tempered by centuries of ocean waves to look quite sculptural.

I had the opportunity to use the trauma room yesterday when we received a radio report about a grass fire, which turned out to be a man on the grass who was on fire. The town was hit with an influx of visitors for the Makah Days Festival, a celebration of Makah culture involving canoe races, traditional dancing, vendors, a talent show, and a salmon bake. In the midst of all the excitement, a large barrel of heated roofing tar spontaneously combusted, and the patient sustained 2nd degree burns on his R hand and R leg. The EMTs brought him in on high-flow oxygen with a nonrebreather mask, already hooked up by IV to a 1-liter bag of normal saline. Although his nasal mucosa was mildly singed, he was breathing normally with no signs of airway edema. The blisters on his skin were starting to pop, and we debrided quite a bit of the dead skin from the burns.
After all the drama, I was able to slip away quietly this morning to meet up with my brother & his family who were camping 54 miles away at the Olympic National Park. We took a trip to La Push to spend the day at Rialto Beach which has a wildly beautiful rocky shoreline punctuated with silvery driftwood that has been tempered by centuries of ocean waves to look quite sculptural.

When I arrived back at Neah Bay just as the sun was setting, I found the entire town shrouded in fog and the main road blocked off by an ambulance, a fire truck, and 2 police cars. Which somehow did not surprise me...
Thursday, August 18, 2011
Neah Bay
 |
| Goodbye, Space Needle! |
 |
| Hello, Bainbridge Island! |
 |
| The shoreline in Neah Bay |
 |
| The Makah Marina |
Whaling was a significant part of ancient Makah tradition, and the tribal logo is a reference to an old legend about a thunderbird delivering a whale to the Makah people during a time of starvation:
You can see representations of this legend in various forms around town:
My temporary home for the next 6 weeks or so is across the street from the police station and jail:
In fact, one of my first clinic patients was a young man in a bright orange jumpsuit, sporting handcuffs and accompanied by a guard. He had pain in both of his forearms, most likely a repetitive stress injury from lifting 60-lb baskets of fish the day before. I suggested releasing the young man ever so briefly from the handcuffs so I could conduct a more thorough exam. This, according to the guard, was not possible. I explained that the repetitive stress injury would resolve faster if the young inmate was allowed to rest from the aggravating activity. The guard shot me a look as if to say, Lady, have you completely lost your marbles?! Apparently there is no rest for the wicked.
Thursday, August 11, 2011
Fly Away With Me
My final night float elicited all kinds of excitement:
-A 77-yr-old woman who had collapsed and was found to have a blood glucose level of 12! After several amps of D50, her blood sugar increased temporarily to 70, then precipitously dropped again. I started her on an intravenous infusion of D10, then ordered some extra D50 for back-up. Turns out the hospital was running low on D50 and had to reserve a few amps for the crash carts. Meanwhile, the patient's blood sugar dropped to 41 despite the D10. Theory: I'm guessing she took some "extra" doses of her extended release glipizide--an insulin secretagogue that can take quite a while to metabolize completely in elderly patients. I ordered glucagon to be administered every time her blood sugar level dropped to the 50s. After 6 or 7 doses, we finally got a blood glucose reading of 124 which fell a bit to 90 an hour later, but managed to stay consistently above 75. By which time, the patient was alert enough to drink juice when prompted.
-A 13-yr-old boy with an impressively large R knee laceration after taking a tumble off his skateboard. The gaping wound revealed some subcutaneous tissue which astounded his parents. You know you're among hunters when the most frequent remark about large lacerations is: "You can see the meat sticking out!" As I was carefully suturing the laceration (13 stitches total), the boy pulled a tiny replica of a skateboard out of his pocket to reenact the scene of the accident for me.
-A cab driver with posterior epistaxis that had been bleeding nonstop for 2 hours, complicated by hypertensive urgency with systolic blood pressures in the 180s. He got a double lumen balloon catheter inserted into his right nasal cavity for tamponade, and several doses of IV labetalol for his blood pressure. Ultimately, he would need to fly to Anchorage for definitive treatment by an ENT specialist.
The funny thing about coming off of night float and taking the morning flight back to Seattle is that almost inevitably you end up on the same Bethel-Anchorage flight as some of your patients! On my flight, I spotted the woman who had the breech delivery in the village (on her way to the NICU in Anchorage to see her newborn), and a little girl who had been treated for R cheek cellulitis secondary to an odontogenic abscess (scheduled for oral surgery in Anchorage later that day). If only the cab driver with the nosebleed had driven us all to the airport and hopped on the flight with us, it would have been a perfect trifecta.
-A 77-yr-old woman who had collapsed and was found to have a blood glucose level of 12! After several amps of D50, her blood sugar increased temporarily to 70, then precipitously dropped again. I started her on an intravenous infusion of D10, then ordered some extra D50 for back-up. Turns out the hospital was running low on D50 and had to reserve a few amps for the crash carts. Meanwhile, the patient's blood sugar dropped to 41 despite the D10. Theory: I'm guessing she took some "extra" doses of her extended release glipizide--an insulin secretagogue that can take quite a while to metabolize completely in elderly patients. I ordered glucagon to be administered every time her blood sugar level dropped to the 50s. After 6 or 7 doses, we finally got a blood glucose reading of 124 which fell a bit to 90 an hour later, but managed to stay consistently above 75. By which time, the patient was alert enough to drink juice when prompted.
-A 13-yr-old boy with an impressively large R knee laceration after taking a tumble off his skateboard. The gaping wound revealed some subcutaneous tissue which astounded his parents. You know you're among hunters when the most frequent remark about large lacerations is: "You can see the meat sticking out!" As I was carefully suturing the laceration (13 stitches total), the boy pulled a tiny replica of a skateboard out of his pocket to reenact the scene of the accident for me.
-A cab driver with posterior epistaxis that had been bleeding nonstop for 2 hours, complicated by hypertensive urgency with systolic blood pressures in the 180s. He got a double lumen balloon catheter inserted into his right nasal cavity for tamponade, and several doses of IV labetalol for his blood pressure. Ultimately, he would need to fly to Anchorage for definitive treatment by an ENT specialist.
The funny thing about coming off of night float and taking the morning flight back to Seattle is that almost inevitably you end up on the same Bethel-Anchorage flight as some of your patients! On my flight, I spotted the woman who had the breech delivery in the village (on her way to the NICU in Anchorage to see her newborn), and a little girl who had been treated for R cheek cellulitis secondary to an odontogenic abscess (scheduled for oral surgery in Anchorage later that day). If only the cab driver with the nosebleed had driven us all to the airport and hopped on the flight with us, it would have been a perfect trifecta.
Tuesday, August 09, 2011
Night of Incredibly Bad OB Mojo
My night float started off with a 24 yr old G1 P0 at 36 + 2/7 wks with her baby in footling breech position, having contractions every 5 minutes, cervix dilated to 2 cm and 60% effaced. We gave her IM terbutaline, but 90 minutes later she had made more cervical change, so high-risk OB came in to attempt an extraversion (to turn the baby around so s/he would be in head-down position). Which failed. Which led to an uneventful C-section that went very well.
After completing several ER admissions (including a 32-yr-old male in diabetic ketoacidosis who was not very compliant with his daily lantus regimen and whose last known HbA1c was a whopping 15.9%; and a tiny 82-yr-old woman with dementia, visual hallucinations, and a 4-night run of insomnia, who promptly fell asleep after 1 mg of haldol) I got a phone call from the village of Emmonak.
Things you never want to hear a health aide say:
1. This woman is having contractions every 3 minutes and she says she's 38 weeks pregnant, but I think she's only 30 weeks pregnant: The patient had no prenatal care for this pregnancy and we had no reliable records of her LMP or even of a positive urine pregnancy test. I started to activate a medevac, thinking that the on-call pediatrician & I would have to fly out to Emmonak for the delivery. I checked her old medical chart and found out she had no history of preterm delivery, just one baby delivered at 37 weeks in 2009.
2. I think her cervix is completely open and I think I can feel the baby's nose: This is a very bad sign that the delivery is imminent and the presenting part is not the head. There's no way the pediatrician & I can get to the village in time.
3. She started pushing, and I think a foot is coming out of her vagina: OMG, it's another footling breech! The health aide had me on speaker phone as I coached him through the breech delivery.
4. The baby is out but he's not breathing: The pediatrician took over the speaker phone and started coaching the health aide & his helpers through the process of neonatal resuscitation.
5. It's been almost 50 minutes and the placenta hasn't come out yet: By this time, the baby was doing better and the pediatrician was en route to Emmonak with the flight crew. The health aide was trying to get pitocin started, as his helpers were applying gentle traction on the umbilical cord and massaging the fundus.
6. Do you think the medevac flight is bringing blood for transfusion?: The health aide estimated a total blood loss of one liter and the mother was still bleeding. The placenta finally came out, and I had the health aide insert his hand in the uterus and manually extract several blood clots and a possible fragment of placenta. I could hear the mother screaming in the background on speaker phone. The only medication for postpartum hemorrhage in the village clinic was methergine which I was hoping not to use. The bleeding finally trickled to a halt, and I had them run IVF at full speed, given mother's tachycardia of 120 bpm.
Meanwhile, I was paged for an OB patient who presented with intractable vomiting, coffee ground emesis and one episode of emesis containing bright red blood, after she drank an entire bottle of R&R the day before. She had been drinking through her entire first trimester, stopped for most of her second trimester, and was now at 26 weeks. I wrote for IV zofran alternating with PR phenergan, then a loading dose of protonix 80 mg by IV, followed by a protonix drip at 8mg/hr to stop the GI bleed. When she complained of epigastric pain, I ordered the magic "GI cocktail" (10cc each of maalox, viscous lidocaine, and benadryl) which soothed her and put her to sleep almost immediately.
Shortly before change of shift, I got a call from the village of Napaskiak: a G3P1 at 34 + 4/7 wks (with excellent dates by 10-wk ultrasound) was having contractions every 3 minutes. After 2 doses of IM terbutaline and a liter of normal saline, the contractions had spaced out a little and were much shorter and less intense. The health aide tried to check the cervix for dilation: "I put my entire hand up there as far as it could go and I still didn't feel anything, " which is a good sign. I spoke with high-risk OB and we agreed to have the pt come to Bethel by boat (just a short 30 minute ride) for further evaluation.
Then I went home and fell, exhausted, into bed.
After completing several ER admissions (including a 32-yr-old male in diabetic ketoacidosis who was not very compliant with his daily lantus regimen and whose last known HbA1c was a whopping 15.9%; and a tiny 82-yr-old woman with dementia, visual hallucinations, and a 4-night run of insomnia, who promptly fell asleep after 1 mg of haldol) I got a phone call from the village of Emmonak.
Things you never want to hear a health aide say:
1. This woman is having contractions every 3 minutes and she says she's 38 weeks pregnant, but I think she's only 30 weeks pregnant: The patient had no prenatal care for this pregnancy and we had no reliable records of her LMP or even of a positive urine pregnancy test. I started to activate a medevac, thinking that the on-call pediatrician & I would have to fly out to Emmonak for the delivery. I checked her old medical chart and found out she had no history of preterm delivery, just one baby delivered at 37 weeks in 2009.
2. I think her cervix is completely open and I think I can feel the baby's nose: This is a very bad sign that the delivery is imminent and the presenting part is not the head. There's no way the pediatrician & I can get to the village in time.
3. She started pushing, and I think a foot is coming out of her vagina: OMG, it's another footling breech! The health aide had me on speaker phone as I coached him through the breech delivery.
4. The baby is out but he's not breathing: The pediatrician took over the speaker phone and started coaching the health aide & his helpers through the process of neonatal resuscitation.
5. It's been almost 50 minutes and the placenta hasn't come out yet: By this time, the baby was doing better and the pediatrician was en route to Emmonak with the flight crew. The health aide was trying to get pitocin started, as his helpers were applying gentle traction on the umbilical cord and massaging the fundus.
6. Do you think the medevac flight is bringing blood for transfusion?: The health aide estimated a total blood loss of one liter and the mother was still bleeding. The placenta finally came out, and I had the health aide insert his hand in the uterus and manually extract several blood clots and a possible fragment of placenta. I could hear the mother screaming in the background on speaker phone. The only medication for postpartum hemorrhage in the village clinic was methergine which I was hoping not to use. The bleeding finally trickled to a halt, and I had them run IVF at full speed, given mother's tachycardia of 120 bpm.
Meanwhile, I was paged for an OB patient who presented with intractable vomiting, coffee ground emesis and one episode of emesis containing bright red blood, after she drank an entire bottle of R&R the day before. She had been drinking through her entire first trimester, stopped for most of her second trimester, and was now at 26 weeks. I wrote for IV zofran alternating with PR phenergan, then a loading dose of protonix 80 mg by IV, followed by a protonix drip at 8mg/hr to stop the GI bleed. When she complained of epigastric pain, I ordered the magic "GI cocktail" (10cc each of maalox, viscous lidocaine, and benadryl) which soothed her and put her to sleep almost immediately.
Shortly before change of shift, I got a call from the village of Napaskiak: a G3P1 at 34 + 4/7 wks (with excellent dates by 10-wk ultrasound) was having contractions every 3 minutes. After 2 doses of IM terbutaline and a liter of normal saline, the contractions had spaced out a little and were much shorter and less intense. The health aide tried to check the cervix for dilation: "I put my entire hand up there as far as it could go and I still didn't feel anything, " which is a good sign. I spoke with high-risk OB and we agreed to have the pt come to Bethel by boat (just a short 30 minute ride) for further evaluation.
Then I went home and fell, exhausted, into bed.
Subscribe to:
Comments (Atom)






















